Talk to a Registered Dietitian and use INSIDER20 for 20% off!
Talk to a real Dietitian for only $99: Schedule Now
This post contains links through which we may earn a small commission should you make a purchase from a brand. This in no way affects our ability to objectively critique the products and brands we review.
Evidence Based Research To fulfill our commitment to bringing our audience accurate and insightful content, our expert writers and medical reviewers rely on carefully curated research.
Read Our Editorial Policy
As one of the most common digestive diseases in the United States, irritable bowel syndrome, or IBS, affects 10% to 15% of American adults.1
With symptoms including bloating or cramping after eating, gas, constipation, or diarrhea, IBS can be an uncomfortable and painful condition that can’t be cured entirely (only managed).
In this article, we’ll detail what IBS is exactly, its symptoms, suspected causes, risk factors, ways to manage it, and food triggers to consider.
Irritable bowel syndrome (IBS) is a common disorder of the digestive tract, causing uncomfortable and painful stomach and bowel symptoms.
There are three primary forms of IBS, including:
In the United States, there is an equal distribution of these diagnoses, whereas IBS-C or IBS-M are more prevalent in Europe than IBS-D.1
Sometimes, a fourth classification is designated, which is called IBS-U (“unclassified”) for someone who doesn’t fit the criteria of the previous three.
Up to 15% of U.S. adults and 10% of adults worldwide have IBS, with women being 1.5 to 2 times more likely to have IBS than men. Women are also more likely to have IBS-C, while men more commonly report IBS-D.1
IBS is a chronic and uncurable condition with treatment based on symptom management, and everyone’s symptoms vary in severity and frequency. Although it can’t be cured, many people can control their IBS symptoms with changes to their diet and lifestyle and, potentially, medication.
IBS symptoms vary widely from person to person, but the main symptoms include:
Less common symptoms may include:
If you have rectal bleeding or bleeding in your stool, you should see a doctor to rule out more serious conditions, like inflammatory bowel disease or colorectal cancer. You should also see a doctor if you have more severe symptoms, unexplained weight loss, or worsening symptoms.
Although it was previously thought that IBS is a “catch-all diagnosis,” meaning doctors would use the term for anyone with digestive symptoms when they couldn’t find anything else wrong, there are some criteria involved in diagnosing someone with IBS.
Much of the time, the first step to diagnosing IBS is still ruling out other gastrointestinal disorders (like inflammatory bowel disease and celiac disease).
From there, the Rome IV Criteria are used to diagnose IBS, which requires recurrent abdominal pain (on average at least one day per week over the past three months) and two or more of the following symptoms:2
The IBS subtypes are then based on someone’s predominant bowel habits on the days of abnormal bowel movements. For example, IBS-C would entail at least 25% of someone’s stools being Bristol Stool Types 1 or 2, while those with IBS-D have at least 25% of their bowel movements as a Bristol 6 or 7.3
However, not everyone fits this criteria, and as there are no clinical biomarkers or blood tests, it can still be challenging to diagnose IBS.
There is no single exact cause of IBS. Many potential causes can trigger symptoms, and someone may have many overlapping root causes that contribute to their IBS.
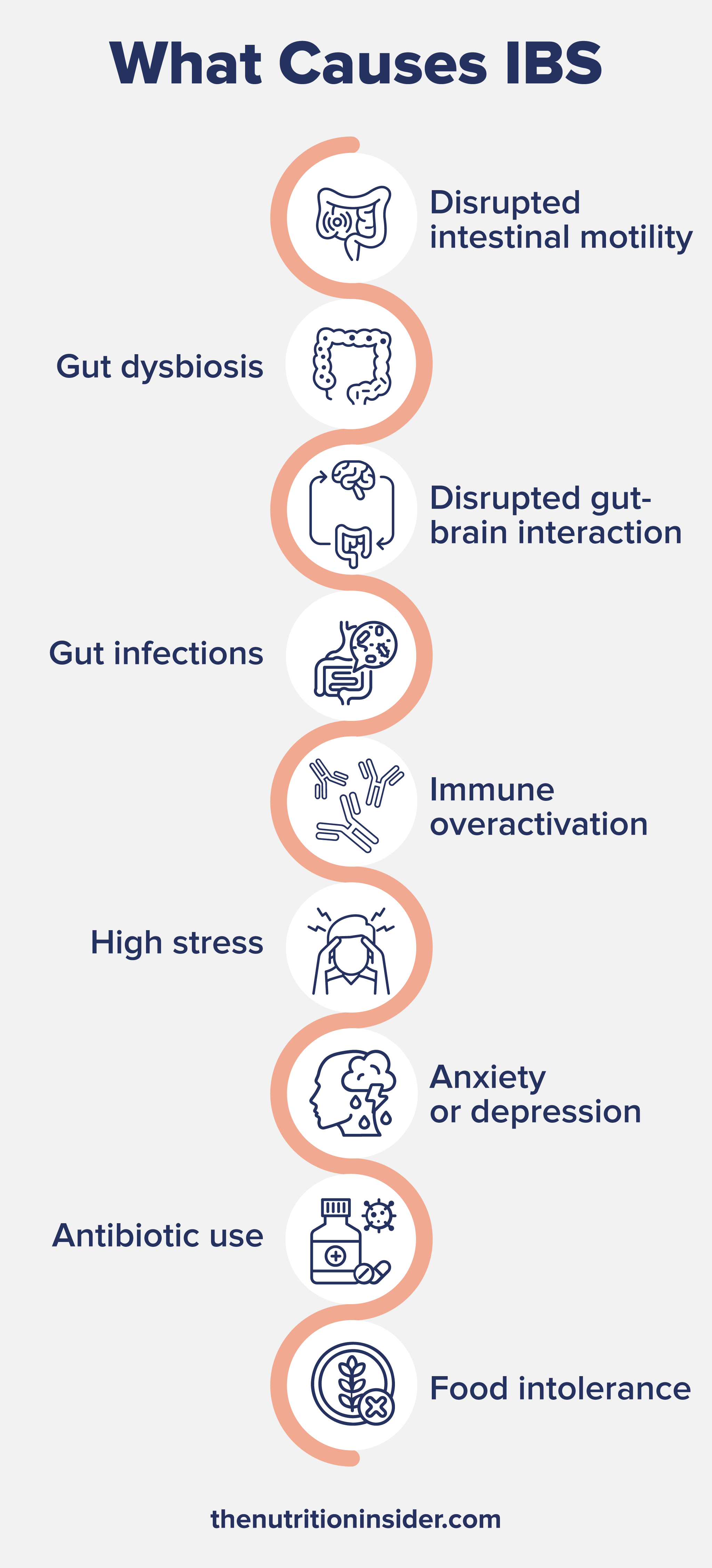
Some causes of IBS include:
Some people are more likely to develop IBS than others. In addition to the conditions mentioned above, risk factors for IBS include:
Foods and beverages to avoid with IBS vary widely from person to person. Keeping a food diary can help you to pinpoint which foods or drinks cause a worsening of symptoms for you.
Some common IBS food triggers may include:
A category of foods called FODMAPs is also a major trigger. FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are sugars in certain foods that the small intestine absorbs poorly.
When FODMAP sugars ferment in the gut of someone with IBS, symptoms like gas, bloating, and cramping can occur. FODMAPs are found in high amounts in foods like garlic, onions, tomatoes, apples, wheat, beans, and more.
In a meta-analysis from 2021, researchers found that people with IBS who followed a low-FODMAP diet had reduced gastrointestinal symptoms and improved quality of life compared to those on a control diet.10
Treatment for irritable bowel syndrome varies depending on your symptoms and suspected causes. For example, someone who has worsening symptoms from high stress and anxiety will have differing treatment and management options than someone who has IBS from eating beans.
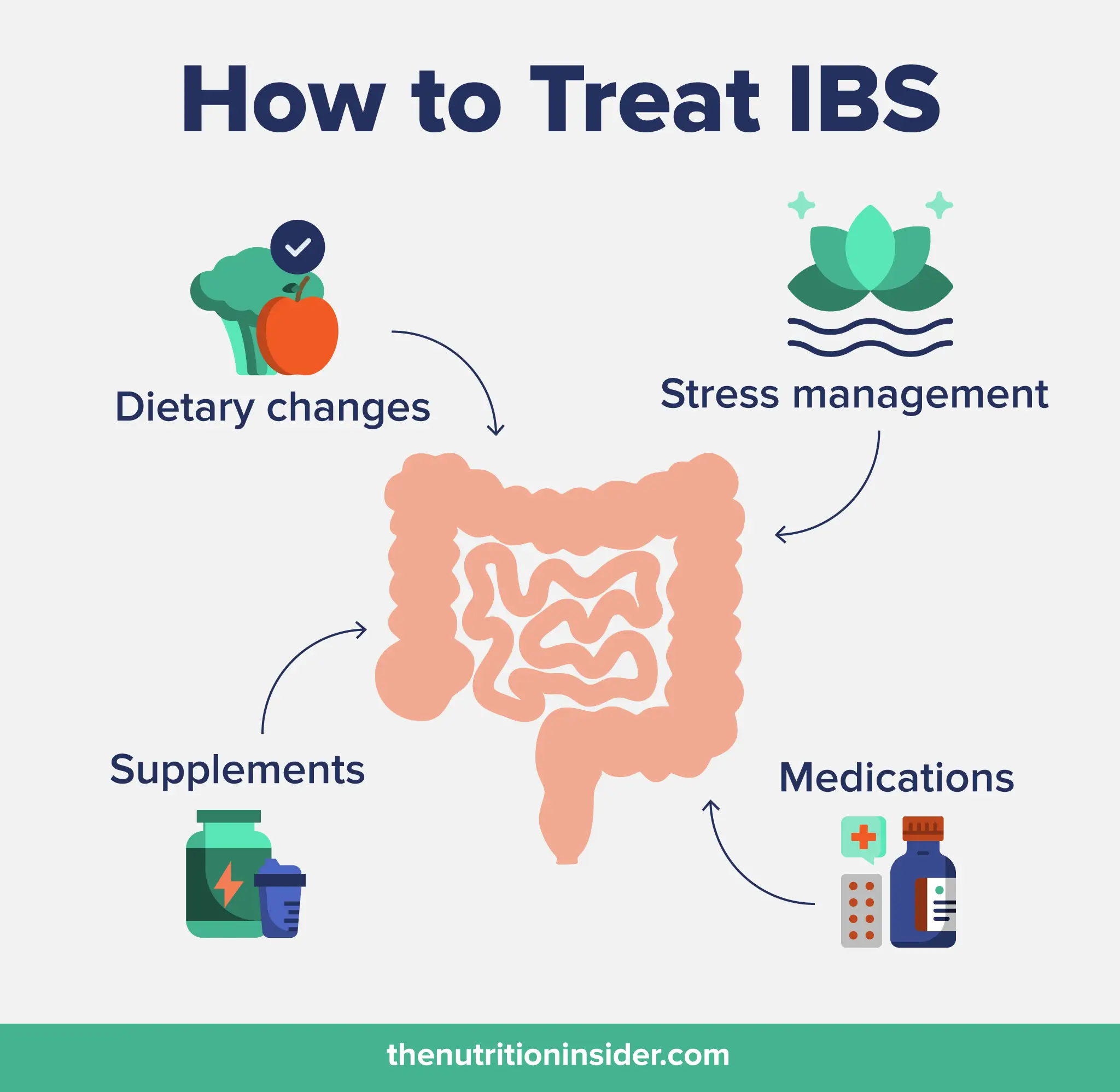
Some of the ways to treat or manage irritable bowel syndrome symptoms include:
As all cases of IBS are different, it takes a lot of trial and error to see what works for you and what does not. Talk to your healthcare provider before starting new digestive supplements.
IBS is not curable, but the symptoms can be managed with diet and lifestyle changes or, in some cases, medications.
Yes, many people with IBS can live completely normal lives. It may take dietary changes, supplements, stress reduction, and sometimes medications to do so.
Foods to avoid with IBS vary widely from person to person. Common IBS triggers include spicy food, beans, legumes, cruciferous vegetables, caffeine, dairy, alcohol, gluten, fried foods, carbonated drinks, and artificial sweeteners. A category of foods called FODMAPs is also a major trigger. FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are sugars in certain foods that the small intestine absorbs poorly. When they ferment in the gut of someone with IBS, symptoms like gas, bloating, and cramping can worsen.
Fixing or managing irritable bowel syndrome can be done with dietary changes (avoiding your personal food triggers), a low-FODMAP diet, stress management, medications (like antidiarrheals or laxatives, depending on your symptoms), and some supplements (like psyllium husk, probiotics, ginger, or peppermint). As all cases of IBS are different, it takes a lot of trial and error to see what works for you and what does not.