Save $40 on your initial consult with a TNI Dietitian!
Talk to a real Dietitian for only $99: Schedule Now
This post contains links through which we may earn a small commission should you make a purchase from a brand. This in no way affects our ability to objectively critique the products and brands we review.
Evidence Based Research To fulfill our commitment to bringing our audience accurate and insightful content, our expert writers and medical reviewers rely on carefully curated research.
Read Our Editorial Policy
You may have heard that colon cancer is becoming more prevalent in younger adults—and it’s true. For the past couple of decades, colorectal cancer rates (which includes cancers of either the colon or rectum) have been steadily increasing in adults under 50.1
While colon cancer was previously thought to affect older adults primarily, younger adults (as young as 20) are now being diagnosed with this form of cancer.2
If you’re in the 20-49 age group and have been concerned about this understandably worrying trend, keep reading to learn more.
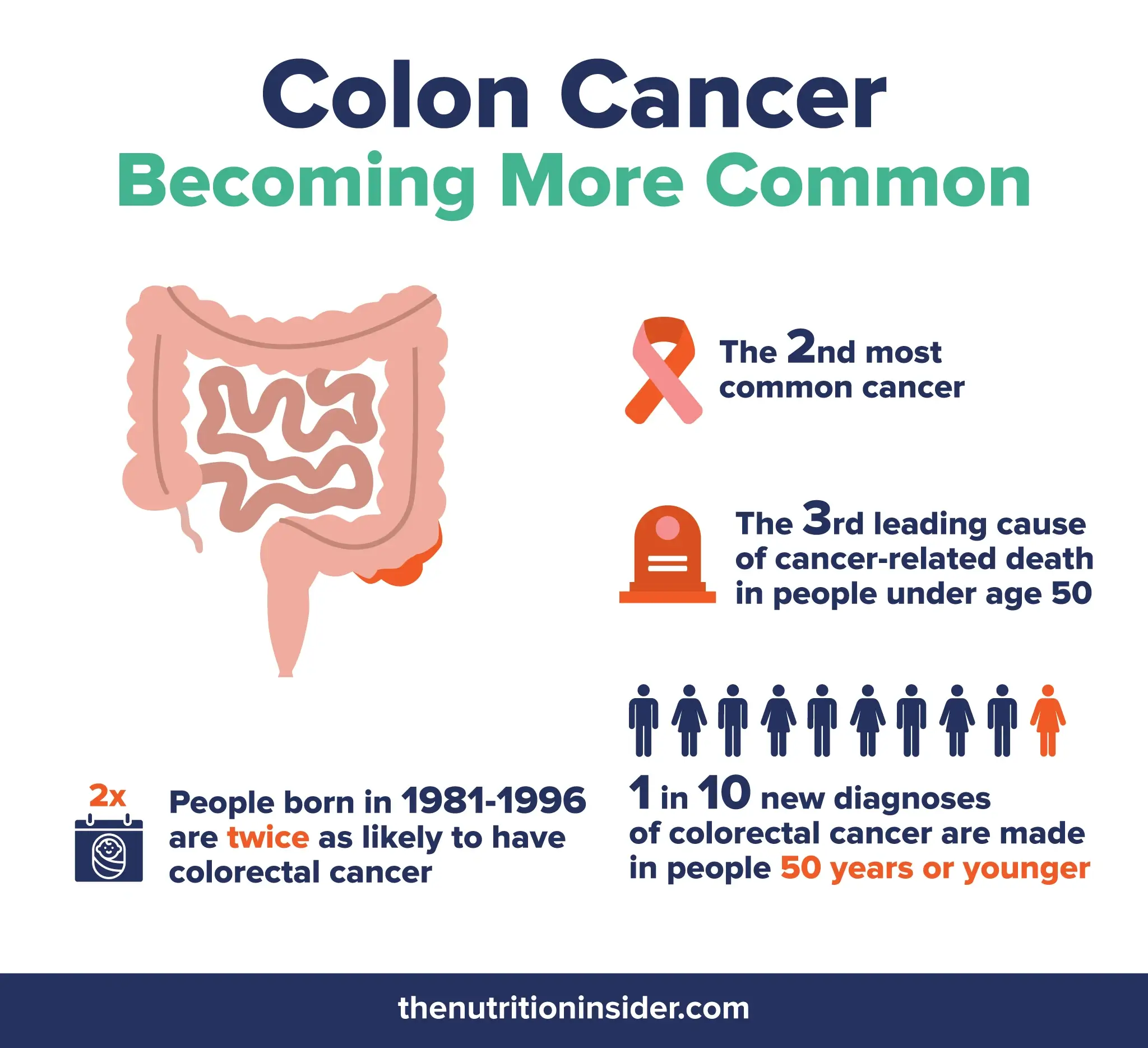
Colorectal cancer is now the second most common cancer and the third leading cause of cancer-related death in people under age 50. According to research from 2020, approximately 1 in 10 new diagnoses of colorectal cancer (CRC) are now made in people 50 years or younger—so much so that it’s now coined “early age onset CRC” (EOCRC).3,4
People who were born between 1981 and 1996 (aka millennials) have a risk of colorectal cancer that is twice as high as people born in 1950.5
And it’s not just in the United States—reports are showing that younger adults in Australia, Canada, New Zealand, the U.K., and countries all over Europe and Asia are experiencing similar increases.6,7
But why exactly is this happening?
To know why colon cancer rates are rising in younger people, let’s take a look at the top risk factors for the disease:8
Although there are other risk factors related to genetics and ethnicity, we’ll focus on these modifiable ones.
As many people know, rates of overweight, obesity, and type 2 diabetes are also having similar upticks in recent decades—especially in younger people.
One study from 2019 found that half of younger adults with colorectal cancer were overweight, and 17% were obese, suggesting a strong association with excess body weight.11
Although smoking is decreasing (especially among young people), alcohol consumption is not. Research shows that even small amounts of alcohol (“light to moderate” drinking) increase the risk of colorectal cancer in a dose-dependent manner (meaning, the more you drink, the greater your risk grows).12
Scientists are also examining the theory that increased environmental pollutants, chemicals in soil and food, and pesticide use contribute to these rising rates.13
Endocrine-disrupting chemicals (which disrupt regular hormonal activity and patterns) may indirectly raise the risk of colorectal cancer by contributing to obesity and metabolic disorders.14
The leading symptoms of colon or colorectal cancer are very similar to many other gastrointestinal disorders, which can make it challenging to know when to see a doctor.
If you see any blood in your stool, that doesn’t mean it’s cancer—but it does mean you should go see your doctor as soon as possible so they can assess you.
According to the CDC, the main symptoms of colon and rectal cancer include:15
Several of these symptoms are common in our daily lives. But if something seems abnormal, go see your doctor.
However, you may not see any symptoms—especially in the early stages—which is why it’s important to follow screening guidelines.

In 2021, health experts started recommending people get colon cancer screenings at age 45, which dropped from the previously recommended age of 50.
Some people should get screened sooner, including those with inflammatory bowel disease (IBD), a personal or family history of colon or rectal cancer, and people with genetic syndromes like familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (Lynch syndrome).
Overall, reducing the modifiable risk factors as much as possible could greatly impact whether or not you develop colon cancer at a young age (or at any age).
These include maintaining a healthy body weight, eating a healthy diet rich in fruits, vegetables, antioxidants, and fiber, exercising, getting your blood sugar under control, monitoring your vitamin D levels, and avoiding smoking and alcohol.