Talk to a Registered Dietitian and use INSIDER20 for 20% off!
Talk to a real Dietitian for only $99: Schedule Now
This post contains links through which we may earn a small commission should you make a purchase from a brand. This in no way affects our ability to objectively critique the products and brands we review.
Evidence Based Research To fulfill our commitment to bringing our audience accurate and insightful content, our expert writers and medical reviewers rely on carefully curated research.
Read Our Editorial Policy
Although it’s best known for its role in bone health, vitamin D does so much more, ranging from mood and muscle strength to cardiovascular health and cognition.
In this article, we’ll explore the top evidence-based health benefits of vitamin D, including what happens if you don’t get enough of it.
Although vitamin D’s classic function is its effects on the skeletal system, it also has anti-inflammatory and immune-regulating properties that can benefit our bones, muscles, brain, lungs, heart, gut, kidneys, and immune system.

Vitamin D first became known for its bone-related benefits when it was discovered as a cure for rickets (while vitamin D deficiency was found to be its cause).
The disease of rickets causes bowed legs and stunted growth because vitamin D helps your body absorb calcium, which induces proper bone mineralization.
In adults, insufficient vitamin D can cause a loss of bone mineral density, bone fractures, osteomalacia (softening of bones), and eventual osteoporosis if untreated.
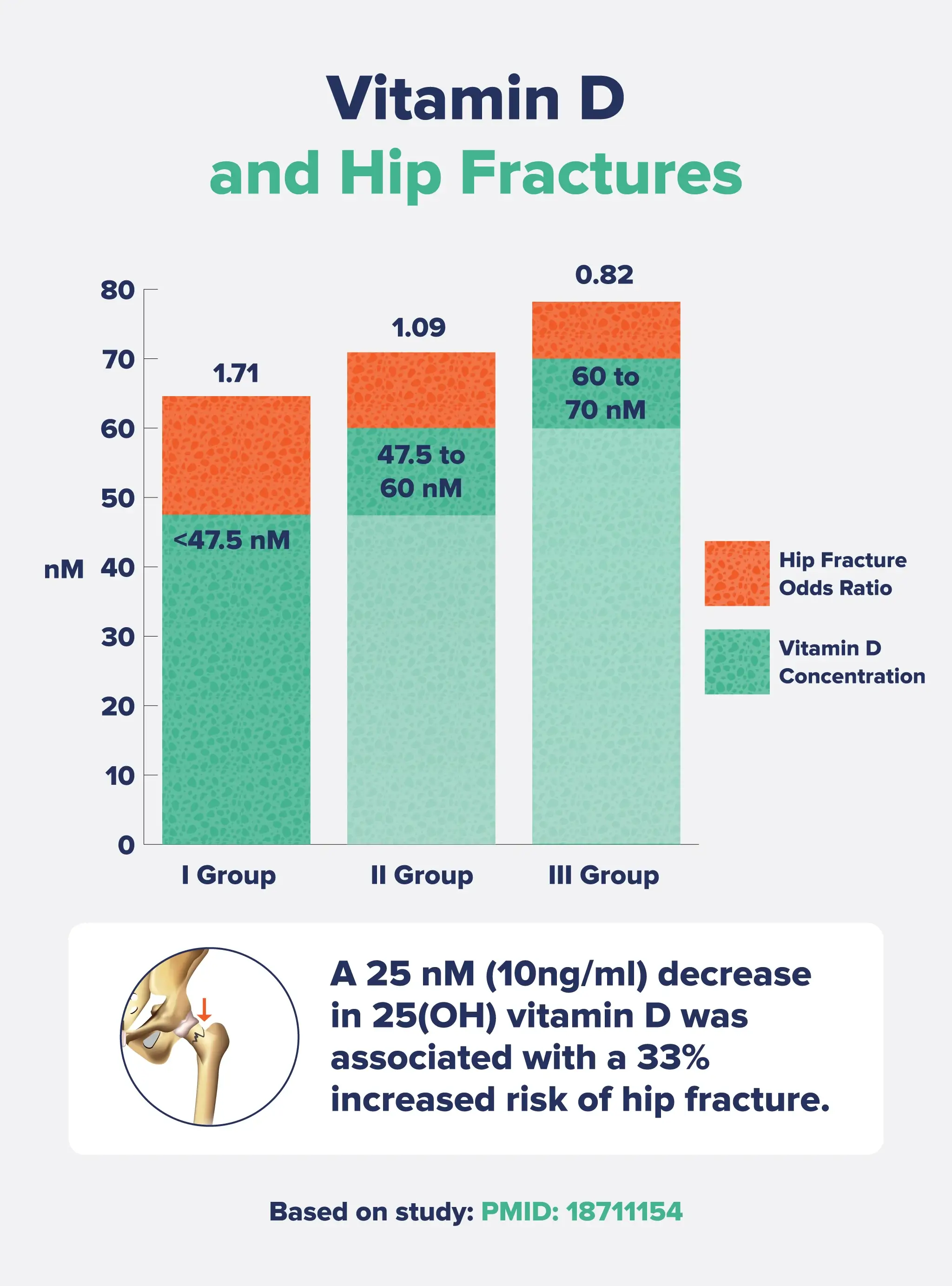
Research with postmenopausal women has found that each 10 ng/mL decrease in blood vitamin D levels is linked to a 33% increased risk of hip fracture.
However, supplementation trials have not consistently shown beneficial effects from taking vitamin D.
For example, a meta-analysis published in the Lancet combined data from 23 studies with over 4,000 people (primarily women). The researchers concluded that only six of the studies significantly and positively affected bone mineral density and only at the femoral neck (at the top of the thigh bone).
Researchers aren’t entirely sure why clinical trials don’t always produce benefits of taking vitamin D. Some theories are inadequate supplement doses, not enough people in the studies being low in vitamin D, studies being too short, or people having poor absorption of the vitamin D supplement.
Vitamin D affects muscle health, as specific vitamin D receptors have been found in skeletal muscle tissue, and vitamin D deficiencies are linked to an increased risk of sarcopenia (muscle wasting) with age.
In a meta-analysis of eight randomized controlled trials, vitamin D supplements in doses of 700-1,000 IU per day reduced the risk of falling among older adults by 19%, which is largely based on muscle strength. Lower doses (200-600 IUs) did not produce any benefit.
Adults who achieved healthy blood vitamin D levels (60 nmol/L or more) also had a 23% reduced risk of falls. While falling doesn’t sound so bad when you’re young, older adults who fall may never fully recover, increasing the risk of fractures, immobility, loss of independence, and even mortality.
Plus, a systematic review of 30 studies concluded that vitamin D supplementation significantly increased muscle strength (but not muscle mass or power), especially in people with low vitamin D levels to begin with and those over the age of 65.However, like with bone strength, not all studies have found that vitamin D improves muscle health—in fact, some research even shows a negative effect.
Sunshine or light therapy has been used to treat depression or mood disorders for centuries, which is likely due, in part, to increased vitamin D levels.
Some potential mechanisms behind vitamin D’s impact on mood include:
In one meta-analysis, researchers found that people who took supplemental vitamin D had significant improvements in their depressive symptoms that were comparable to anti-depressant medication.
Notably, these results were only from high-quality trials, meaning the researchers excluded poorly designed studies with low methodological quality. When they analyzed low-quality studies, the results were either null or negative, emphasizing how poorly designed studies can affect supplementation trials—which may be why so many other trials do not find benefits.
Having adequate vitamin D levels is associated with a reduced risk of several respiratory illnesses, including tuberculosis, influenza, and upper respiratory tract infections.
In a meta-analysis analyzing data from almost 11,000 participants, people who took vitamin D supplements had a 19% reduced risk of acute respiratory tract infections, with the most significant benefits in vitamin D deficient people. One theory behind vitamin D’s link to respiratory health is that it increases the production of antimicrobial peptides, which fight against respiratory pathogens and help regulate local immune and inflammatory responses.
Vitamin D may benefit cardiovascular health by suppressing foam cell formation. Foam cells are pro-inflammatory, cholesterol-containing macrophage cells that increase fatty deposits on blood vessel walls, contributing to heart disease.
Research has also shown that vitamin D plays a role in cholesterol and blood pressure regulation, glucose metabolism, and insulin sensitivity, all of which are important markers of heart health.
In a large study of over 41,000 adults, vitamin D deficiency was linked to an increased risk of coronary artery disease, heart failure, stroke, and heart attack. In addition, people with the lowest vitamin D levels were most likely to have other cardiometabolic-related conditions or symptoms, including a higher prevalence of diabetes, hypertension, hyperlipidemia, and peripheral vascular disease. Another study of over 21,000 older adults found that vitamin D supplements (a monthly dose of 60,000 IUs for 5 years) slightly reduced the incidence of major cardiovascular events, particularly heart attacks.
Low vitamin D levels have also been associated with cognitive impairment and dementia.
The link between vitamin D and cognition is similar to that between vitamin D and mood. Vitamin D reduces neuroinflammation and provides neuroprotective activity.
Research suggests that vitamin D promotes the production of neurotrophic factors such as nerve growth factor (NGF), which, as the name suggests, regulates the growth and maintenance of neurons. While observational studies and meta-analyses have consistently shown lower vitamin D levels in people with Alzheimer’s disease and other forms of cognitive impairment, supplementation trials have produced mixed results.
With its anti-inflammatory and immunomodulatory properties, vitamin D may support a healthy gut.
Vitamin D increases the production of antimicrobial peptides and improves the innate immune response in the gut, which can help to reduce dysbiosis and support a healthy gut microbiome. It may also support gut integrity by strengthening the tight junctions in the epithelial lining of the gut, which is linked to reduced intestinal permeability. Plus, vitamin D deficiency is associated with an increased risk of inflammatory bowel disease (Crohn’s disease and ulcerative colitis) and improvements in symptoms related to IBD.
Vitamin D deficiency is linked to decreased kidney function, and people with chronic kidney disease have been shown to have altered vitamin D metabolism.
This is because the kidneys convert the inactive form of vitamin D into the active form, which can further decrease vitamin D levels in people with chronic kidney disease.
Vitamin D plays a role in both innate and adaptive immune responses.
Briefly, the innate immune system is the first line of defense against invading bacteria or pathogens. In contrast, the adaptive immune system is more specialized, targeting specific invaders and adapting to previous infections.
Vitamin D facilitates innate immunity by enhancing the production of the molecule cathelicidin (one of those antimicrobial peptides mentioned previously) and defensive immune cells, as well as strengthening the physical barrier function of epithelial cells.
It also modulates the adaptive immune system by supporting the differentiation of naive T cells into immune-benefiting regulatory T cells and reducing the secretion of pro-inflammatory cytokines.
Because of these immunomodulatory effects, vitamin D has been studied for its role in reducing the incidence of or controlling the symptoms of certain autoimmune diseases, including rheumatoid arthritis, lupus, psoriasis, and multiple sclerosis. Notably, an extensive study of almost 26,000 people found that vitamin D supplements (2,000 IUs per day for five years) reduced the rate of developing any autoimmune disease by 22%.
There are many potential symptoms of inadequate or deficient vitamin D, including:
• Fatigue or constant low energy
• Getting sick frequently
• Depression or mood disorders
• Joint, muscle, or bone pain
• Slow wound healing
• A tingly sensation in the hands or feet
• Bowed legs (when the deficiency is severe, causing rickets)
Your doctor will probably recommend vitamin D supplements if you have low vitamin D levels (as verified by a lab test). Taking vitamin D supplements (especially in higher doses) is not recommended without knowing your blood levels.
That said, most people’s vitamin D intake from diet is low (even when adding in fortified foods), and we may not get enough vitamin D from sun exposure, either. Factors like sunscreen usage, lots of time spent indoors, the latitude where you live, your weight, genetics, and skin color all affect how much vitamin D we can make from sunshine and, therefore, whether you need vitamin D supplements. However, we can’t tell you if you need vitamin D supplements, so head to your doctor!
Vitamin D is a fat-soluble vitamin, meaning it gets stored in our bodies and does not get excreted through urine (like water-soluble vitamins do). Therefore, vitamin D toxicity is possible from taking excess vitamin D. You can’t overdose on vitamin D from the sun, but you can take too much in supplemental form and develop vitamin D toxicity or other adverse effects.
Taking too much vitamin D causes hypercalcemia (high calcium levels in the blood), which leads to symptoms like nausea, vomiting, muscle weakness, neuropsychiatric disturbances, pain, loss of appetite, dehydration, polyuria, excessive thirst, and kidney stones or other kidney problems.
Extreme vitamin D toxicity can cause renal (kidney) failure, calcification of the heart, cardiac arrhythmias, and even death.
The NIH has set the UL (Tolerable Upper Intake Level) for vitamin D for adults at 100 mcg (4,000 IU) per day. However, they also state that symptoms of toxicity are “unlikely at daily intakes below 10,000 IU.” If you have a vitamin D deficiency, your doctor may prescribe doses higher than the UL for a short period to increase your levels.
It doesn’t matter if you take vitamin D in the morning or at night. However, as it is a fat-soluble vitamin, you should take it with food to increase its absorption.
The recommended dietary allowance (RDA) for vitamin D is 600 IU for adults up to age 70 and 800 IU for adults over 70, with a serum vitamin D level of 20 ng/mL considered adequate.
However, many researchers think that the current RDA needs to be set higher. For example, The Endocrine Society states that vitamin D levels in the blood should be above 30 ng/mL, requiring 1,500-2,000 IU per day for adults to maintain these levels.
Many studies show that vitamin D3 supplements in the range of 1,000 to 4,000 IU per day are safe and beneficial, with some research showing that up to 8,000 IU per day is safe for a shorter period in adults with vitamin D deficiency.
However, it’s essential to know your vitamin D levels before taking supplements in high doses of vitamin D above the RDA, so see your doctor for labwork first.