This post contains links through which we may earn a small commission should you make a purchase from a brand. This in no way affects our ability to objectively critique the products and brands we review.
Sunlight and Mental Health: What’s the Link?
Evidence Based Research To fulfill our commitment to bringing our audience accurate and insightful content, our expert writers and medical reviewers rely on carefully curated research.
Read Our Editorial Policy
As anyone dealing with seasonal depression can attest, sunshine—or lack thereof—can have significant effects on our mood.
But as millions of U.S. adults experience mental illness or low mood year-round, sunlight exposure may be able to help improve some of the symptoms—let’s take a closer look at sun therapy and how it can help you.
Sun Exposure and Mental Health
Many adults experience mental illness, low mood, or changes to mental health—can sun exposure help?
Sunlight and Mood Disorders
A lack of sun exposure is one reason why people develop Seasonal Affective Disorder (often referred to as seasonal depression or SAD).
SAD is a mood disorder characterized by depressive symptoms that increase during the winter months and can be helped with light therapy.
Plus, the change in season and loss of sun can disrupt the balance of the body’s level of melatonin, which is a hormone involved in both sleep and mood.
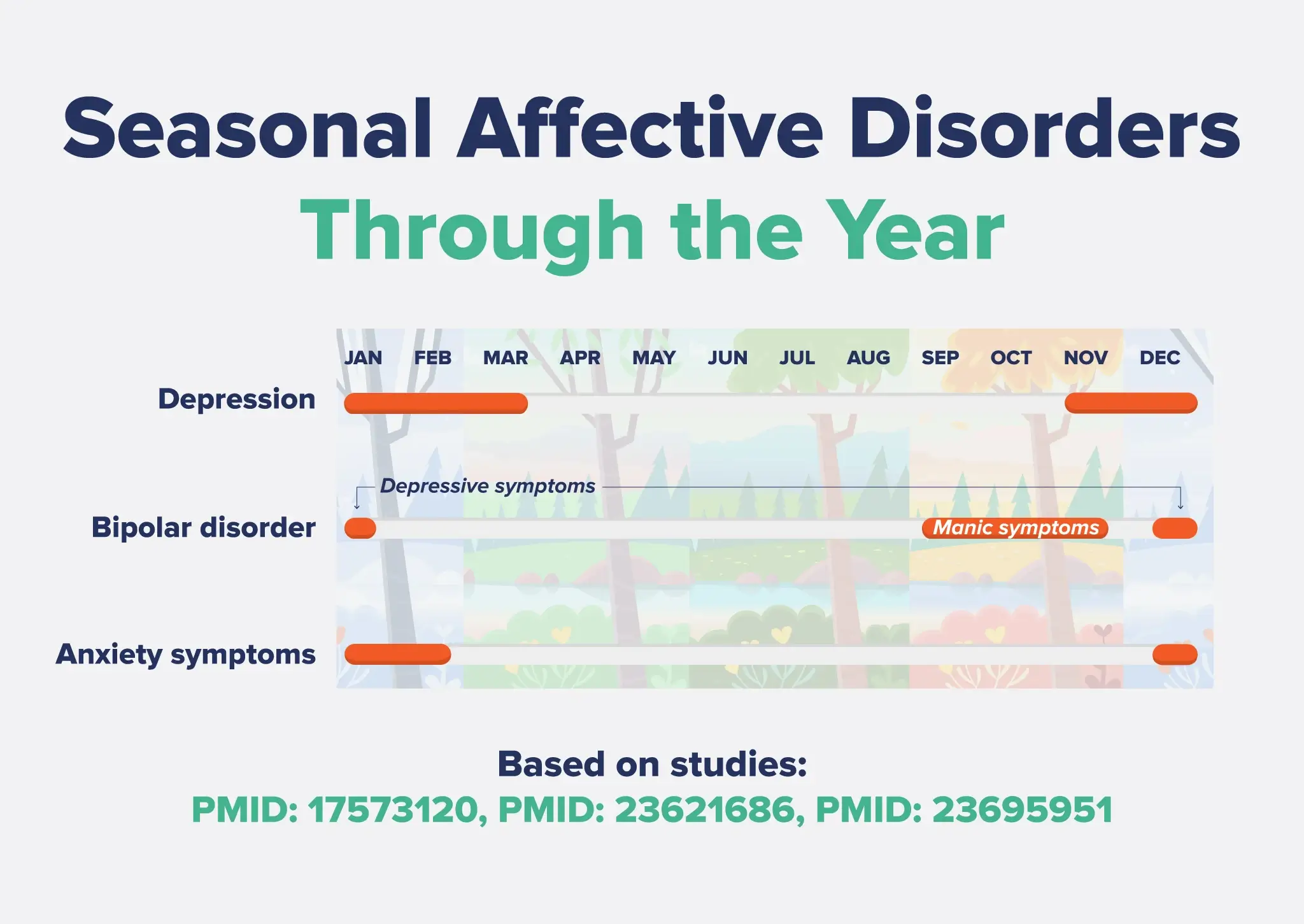
Research with over 10,000 men and women in Norway found a significant seasonal effect on mood disorders, with higher levels of depression (also known as major depressive disorder or MDD) from November to March.1
Bipolar disorder also displays seasonal variations. A smaller study of 314 people with bipolar disorder found that hypomanic and manic symptoms peaked in the fall, while depressive symptoms peaked around the time of the winter solstice.2
Similarly, research out of the Netherlands showed that anxiety symptoms were more prevalent during the winter months.3
Getting enough natural light improves the mood of office employees who ordinarily see artificial light all day. In this research, workers exposed to sunlight and natural elements during the workday reported reduced depression and anxiety and increased job satisfaction.4
Another study looked at the mental health status of operating room nurses who worked long hours without seeing much sunlight.5
The researchers found that nurses who saw the least amount of sunlight were most likely to have worse mental health, including anxiety, depression, and psychological distress. Conversely, as nurses increased their time in natural light, their mental health and well-being improved.5
Keep in mind that depression treatment needs to be monitored by doctors, and you should never quit your anxiety or depression treatment without first speaking with a professional.
Sunlight and Serotonin
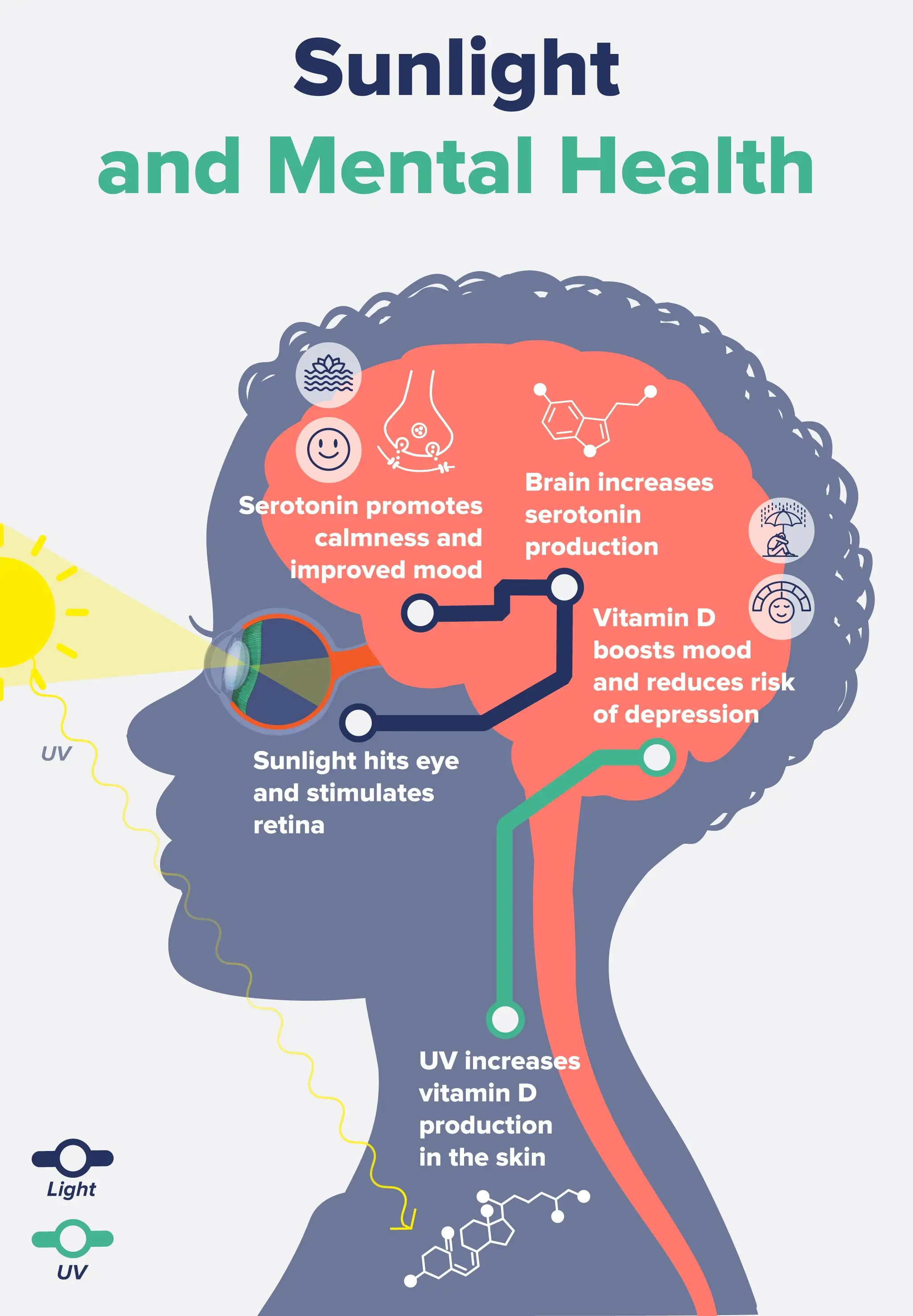
The link between sunlight and mental health is likely mediated by serotonin.
Exposure to sunshine increases serotonin levels, our primary “feel-good” neurotransmitter, which promotes calmness and improved mood.
When sunlight enters your eyes, it stimulates the retina to cue your brain to produce serotonin.
Serotonin is found in the brain, retina, and gut, as well as in human cutaneous (skin) tissue. Studies have shown that the epidermis and dermis express enzymes needed to transform the amino acid tryptophan into 5-HTP—the precursor to serotonin.6
Serotonin also exhibits natural seasonal variation in the central nervous system, and its levels have been shown to be lowest in the winter.7
The research on serotonin’s involvement in mood disorders like depression is conflicting, with some studies showing that a lack of serotonin drives depression, while others show no connection.8,9
Sunlight and Vitamin D
Natural light also increases vitamin D production in the skin, and higher vitamin D levels are linked to a healthier mood and reduced risk of depression.10
Dozens of studies have found that people with depression had lower levels of vitamin D compared to those without, and those with the lowest vitamin D levels had the greatest risk of depression.11
However, vitamin D supplementation trials do not always produce beneficial effects on depression, suggesting that sunshine may be a better route for boosting both vitamin D status and mood.
How to Safely Get Sun Exposure for Mental Health
If you want to use sunlight or light therapy for anxiety or depression treatment or to help treat another mental illness, be sure to speak with your doctor first.
To safely get sun exposure, don’t go outside without sun protection for more than 10 to 15 minutes, or possibly less if you have fair skin. People with fair skin are at higher risk of developing adverse effects from more sun exposure.
Avoid going outside without sun protection during the peak hours of the day when the sun’s damaging rays are strongest, typically between 10 a.m. and 4 p.m.
Other sun safety tips include:
- Wear sunscreen. Use a broad-spectrum sunscreen of SPF 30 or more that protects against both UVA and UVB rays. You should be applying sunscreen every two hours or more often if you go swimming or are sweating. Use mineral-based sunscreen with ingredients like zinc oxide or titanium dioxide that physically reflect UV rays. Don’t forget your scalp, ears, back of neck, and lips (use an SPF chapstick). Don’t be fooled if it’s cloudy out—wear sunscreen in all weather.
- Wear protective clothing. Shirts with long sleeves, pants, wide-brimmed hats, and sunglasses can protect you from the sun during outdoor activities. Look for protective clothing with a UV protection factor (UPF) or made of a tightly woven fabric.
- Avoid tanning beds. It’s not the 2000s anymore; no one should be using a tanning bed! Enough said.
- Seek shade. Use umbrellas or seek other sources of shade to provide additional sun protection during the hottest part of the day.
- Be aware of your medications. Many over-the-counter and prescription medicines increase the skin’s sensitivity to UV rays, so be aware of their side effects on light sensitivity. Some medications that increase sun sensitivity include certain antibiotics, birth control pills, topical benzoyl peroxide, retinol, and most other “active” skincare products.
Light Therapy for Mental Health
If you live in a more northern latitude or cannot get sun exposure each day, light therapy is another option.
Also known as sun lamp therapy or phototherapy, light therapy involves sitting in front of a light box that emits a bright light of 10,000 lux (a measure of light intensity) or for about 30 minutes each day.
Research combining data from 19 studies found that bright light therapy is better than a placebo at reducing symptoms of Seasonal Affective Disorder. However, they conclude that larger clinical trials are needed.12
Ideally, you’d use the lightbox when you wake up, as this can also help regulate your circadian rhythm. You shouldn’t stare directly at the bright light lamp, and it’s typically recommended that you sit 16 inches from it.13
Sun Therapy FAQs
Can lack of sunlight increase anxiety?
Yes, a lack of adequate sunlight exposure could potentially increase anxiety. As over 40 million U.S. adults experience anxiety at some point, increasing sun exposure may be able to help.
How does light affect mental health?
Sunlight is thought to have positive outcomes on mental health and well-being, including mood, depression, anxiety, and mental alertness. If you have a severe mental disorder or take medications, always speak with your doctor first before trying something new, and never stop taking your medications on your own. Sunlight is not a replacement for depression treatment, but it may help with delivering positive outcomes.
How does sunlight increase serotonin?
When sunlight hits your eyes, the UV rays trigger the retina to cue your brain to make serotonin. Serotonin is found in the brain, retina, and gut, as well as in human cutaneous (skin) tissue. Studies have shown that the epidermis and dermis express enzymes needed to transform the amino acid tryptophan into 5-HTP—the precursor to serotonin.
What are the benefits of sun lamp therapy?
The benefits of sun lamp therapy are similar to actual sunshine, including improvements in seasonal depression (SAD), major depressive disorder, and low mood. Light therapy can also help to regulate the circadian rhythm, which is linked to better sleep, metabolic health, heart health, cognitive function, and more.
- Oyane, N. M., Bjelland, I., Pallesen, S., Holsten, F., & Bjorvatn, B. (2008). Seasonality is associated with anxiety and depression: the Hordaland health study. Journal of affective disorders, 105(1-3), 147–155. https://doi.org/10.1016/j.jad.2007.05.002
- Akhter, A., Fiedorowicz, J. G., Zhang, T., Potash, J. B., Cavanaugh, J., Solomon, D. A., & Coryell, W. H. (2013). Seasonal variation of manic and depressive symptoms in bipolar disorder. Bipolar disorders, 15(4), 377–384. https://doi.org/10.1111/bdi.12072
- Winthorst, W. H., Roest, A. M., Bos, E. H., Meesters, Y., Penninx, B. W., Nolen, W. A., & de Jonge, P. (2014). Self-attributed seasonality of mood and behavior: a report from the Netherlands study of depression and anxiety. Depression and anxiety, 31(6), 517–523. https://doi.org/10.1002/da.22130
- An, M., Colarelli, S. M., O’Brien, K., & Boyajian, M. E. (2016). Why We Need More Nature at Work: Effects of Natural Elements and Sunlight on Employee Mental Health and Work Attitudes. PloS one, 11(5), e0155614. https://doi.org/10.1371/journal.pone.0155614
- Wang, J., Wei, Z., Yao, N., Li, C., & Sun, L. (2023). Association Between Sun Exposure and Mental Health: Evidence from a Special Population Without Sunlight in Work. Risk management and healthcare policy, 16, 1049–1057. https://doi.org/10.2147/RMHP.S420018
- Nordlind, K., Azmitia, E. C., & Slominski, A. (2008). The skin as a mirror of the soul: exploring the possible roles of serotonin. Experimental dermatology, 17(4), 301–311. https://doi.org/10.1111/j.1600-0625.2007.00670.x
- Sansone, R. A., & Sansone, L. A. (2013). Sunshine, serotonin, and skin: a partial explanation for seasonal patterns in psychopathology?. Innovations in clinical neuroscience, 10(7-8), 20–24.
- Pannu, A., & K Goyal, R. (2023). Serotonin and Depression: Scrutiny of New Targets for Future Anti- Depressant Drug Development. Current drug targets, 24(10), 816–837. https://doi.org/10.2174/1389450124666230425233727
- Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2023). The serotonin theory of depression: a systematic umbrella review of the evidence. Molecular psychiatry, 28(8), 3243–3256. https://doi.org/10.1038/s41380-022-01661-0
- Hoang, M. T., Defina, L. F., Willis, B. L., Leonard, D. S., Weiner, M. F., & Brown, E. S. (2011). Association between low serum 25-hydroxyvitamin D and depression in a large sample of healthy adults: the Cooper Center longitudinal study. Mayo Clinic proceedings, 86(11), 1050–1055. https://doi.org/10.4065/mcp.2011.0208
- Menon, V., Kar, S. K., Suthar, N., & Nebhinani, N. (2020). Vitamin D and Depression: A Critical Appraisal of the Evidence and Future Directions. Indian journal of psychological medicine, 42(1), 11–21. https://doi.org/10.4103/IJPSYM.IJPSYM_160_19
- Pjrek, E., Friedrich, M. E., Cambioli, L., Dold, M., Jäger, F., Komorowski, A., Lanzenberger, R., Kasper, S., & Winkler, D. (2020). The Efficacy of Light Therapy in the Treatment of Seasonal Affective Disorder: A Meta-Analysis of Randomized Controlled Trials. Psychotherapy and psychosomatics, 89(1), 17–24. https://doi.org/10.1159/000502891
- Levitan R. D. (2005). What is the optimal implementation of bright light therapy for seasonal affective disorder (SAD)?. Journal of psychiatry & neuroscience : JPN, 30(1), 72.








