This post contains links through which we may earn a small commission should you make a purchase from a brand. This in no way affects our ability to objectively critique the products and brands we review.
Leaky Gut Syndrome: Symptoms, Causes, and Treatments
Evidence Based Research To fulfill our commitment to bringing our audience accurate and insightful content, our expert writers and medical reviewers rely on carefully curated research.
Read Our Editorial Policy
Leaky gut syndrome, or intestinal hyperpermeability, has gained much more attention in the past two decades—despite some debate about whether or not it is an actual condition.
Leaky gut syndrome is thought to cause digestive symptoms, trigger inflammation, and contribute to a wide variety of health issues, ranging from acne and arthritis to migraines and metabolic syndrome.
But what is leaky gut, exactly? And what causes it? In this article, we’ll answer these questions and more, including ways to treat it with supplements and nutrition.
What Is Leaky Gut Syndrome?
The more scientific term for leaky gut is “increased intestinal permeability” or “intestinal hyperpermeability,” meaning that a part of the small and large intestines becomes excessively permeable.
Leaky gut is thought to occur when the one-cell-thick layer of epithelial cells lining the intestines becomes “leaky” with growing gaps between the cells.
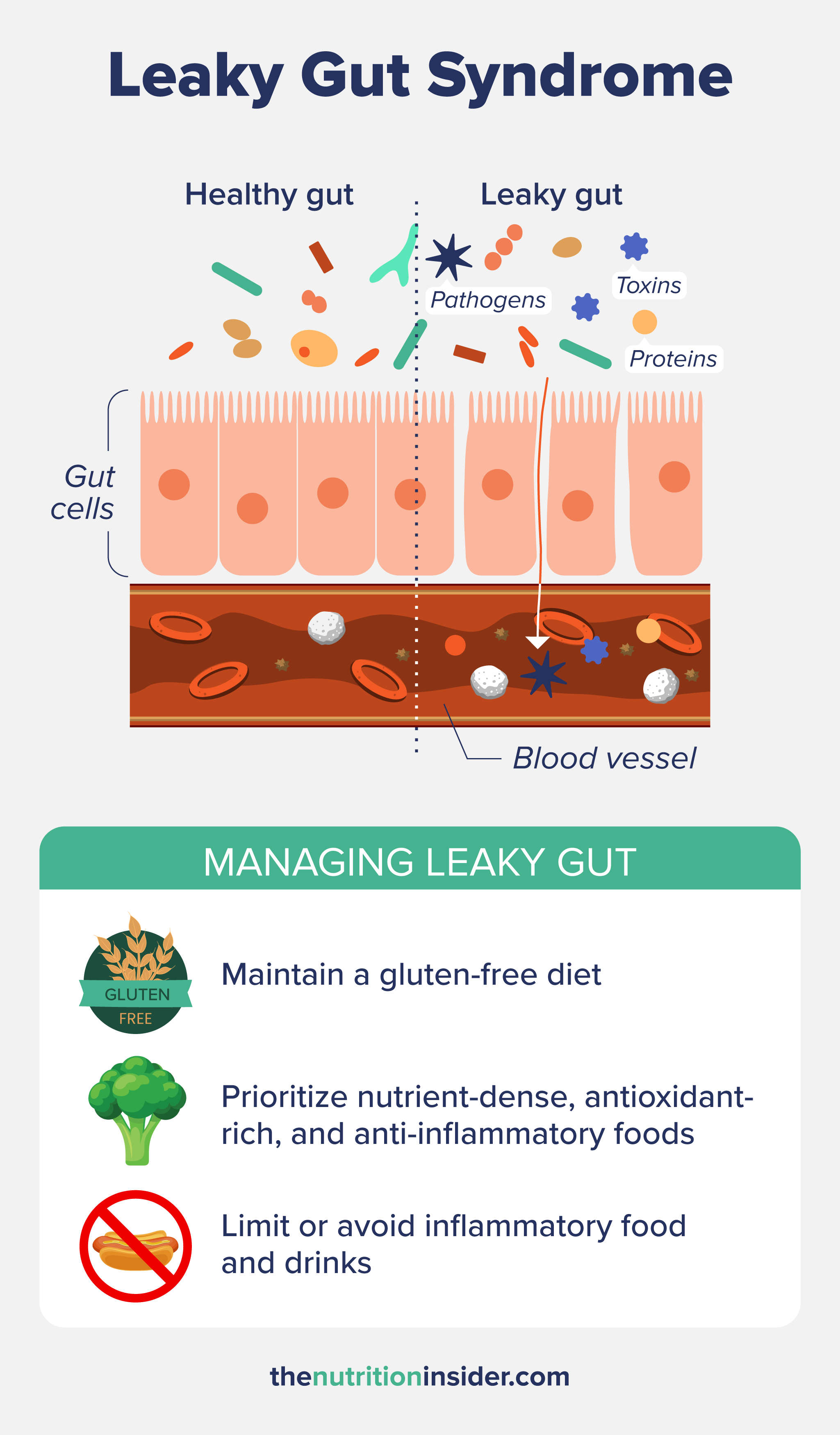
When this happens, the excessive permeability may allow toxins, pathogens, or proteins to travel out of the digestive tract into the bloodstream. This is thought to contribute to a myriad of health issues, although the research isn’t always conclusive.
Here’s what we do know: our intestinal barrier lining is only one cell thick, made up of epithelial cells that are constantly renewing themselves. We need a strong and tight intestinal barrier to control what enters the bloodstream and what stays inside the gut.
Epithelial cells in the intestinal lining are “sealed” together by protein complexes called tight junctions, which act like a physical barrier between the gut and the bloodstream.
Essentially, tight junctions are gatekeepers between the bloodstream and gut, allowing water and nutrients to pass through but keeping out toxins, most proteins, and pathogens from entering. If the gaps between tight junctions start to become too big, the stuff we want to keep in our guts (typically to be eliminated) can escape (i.e., “leak”) into the rest of the body.
When too-big proteins and toxins enter the bloodstream, the body’s immune response is activated to deal with the invader. This elevates inflammation and is thought to contribute to chronic diseases related to inflammation (which are just about all of them).
The gut lining also uses another barrier to keep things out, which is made up of mucus, immune cells, antimicrobial peptides, and a gel-like coating of proteins called the glycocalyx. These molecules create a sticky surface that physically traps harmful pathogens or chemically prevents them from adhering to epithelial cells. In addition to increasing gaps between tight junctions causing leaky gut, dysfunction in this mucosal barrier is also implicated in intestinal permeability.
But what causes these mechanisms to break down in the first place? Let’s take a look.
What Causes Leaky Gut Syndrome?
Although the term “leaky gut” has been found in the scientific literature as far back as the 1970s, researchers are still trying to figure out exactly what causes it. Like many gut-related conditions, there are many potential causes of leaky gut.
In 2000, Dr. Alessio Fasano and his team discovered a protein called zonulin that regulates the permeability of the intestines.1
Elevated zonulin levels cause the tight junctions between intestinal epithelial cells to open up too much, creating the characteristic gaps of leaky gut. Two conditions that cause zonulin activation are dysbiosis—excessive harmful bacteria in the gut microbiome and too few healthy ones—and gluten consumption in sensitive people.
Some other contributing factors that contribute to leaky gut include:
- Having excess body fat: Excess body fat is linked to elevated levels of a harmful bacterial toxin called lipopolysaccharide (LPS) in the bloodstream, which travels through permeable tight junctions to cause inflammation in the body.2
- Excessive alcohol consumption: Alcohol promotes gut dysbiosis and harmful bacteria overgrowth. It also increases the release of endotoxins produced by certain types of bacteria that can aggravate the intestinal mucosa of the gut lining.
- Chronic stress: Stress and mental health conditions like anxiety and depression can all increase gut barrier permeability.
- Chronic use of antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) (like aspirin and ibuprofen) can cause gut dysbiosis
- Chronic inflammation: Chronic inflammation can be caused by many things, including obesity, alcohol consumption, chronic stress, and an unhealthy diet.
- Gluten consumption: In some people, gluten will trigger zonulin to create gaps in the intestinal tissue. While some researchers think that eating gluten can cause leaky gut in everybody, others believe that genetics make only some people susceptible to gluten-induced leaky gut.
- Other digestive conditions: Conditions such as inflammatory bowel disease (IBD), irritable bowel syndrome, and celiac disease, and intestinal infections like H. pylori can also contribute.
- Poor diet: This can include nutrient deficiencies, high-fat intake, and excessive sugar consumption, as fructose can harm the barrier function of the intestinal wall. Artificial sweeteners, preservatives, and colors can also contribute to poor gut health.
Symptoms of Leaky Gut Syndrome
The most apparent symptoms of leaky gut are digestive-related, including bloating, gas, cramping, abdominal pain, constipation, or diarrhea.
There are also potential non-digestive symptoms or conditions associated with leaky gut, including:
- Fatigue or chronic fatigue syndrome
- Mood and mental health disorders like anxiety and depression
- Autoimmune diseases, including type 1 diabetes, multiple sclerosis, rheumatoid arthritis, and celiac disease3-6
- Food intolerances
- Allergies and asthma
- Skin issues like acne, rashes, and eczema
- Insulin resistance and metabolic problems
However, it can be difficult to determine if leaky gut causes these conditions or is a symptom of them. Some research with animals has found that increased intestinal permeability occurs before the onset of some diseases, including type 1 diabetes, celiac disease, and IBS, suggesting that leaky gut can, in fact, be the cause rather than the symptom in some cases.7,8
Treating Leaky Gut Syndrome
There is no single gold standard for treating leaky gut, but targeting its root cause is a first step. A functional medicine practitioner can help you figure out what is causing your elevated intestinal permeability.
Some ways to treat leaky gut may include correcting gut dysbiosis, reducing inflammation, improving diet, treating digestive conditions, managing body weight, or reducing stress.
Prebiotics
Prebiotics are types of dietary fiber that provide fuel for intestinal cells in the form of short-chain fatty acids. They also benefit the leaky gut by strengthening the gut barrier, increasing the growth of healthy bacteria, and supporting healthy immune cell functioning.
Prebiotics can come in supplemental or food forms, such as garlic, onions, leeks, asparagus, and chicory. One study found that people who increased their daily fiber intake from 19 grams to 29 grams had significantly reduced zonulin levels over the six-month study. Zonulin tests are one of the main ways to test for intestinal permeability.9
It’s thought that soluble fiber especially helps leaky gut because the intestinal fermentation of soluble fiber boosts butyrate production, which strengthens intestinal barrier function.
Probiotics
As gut dysbiosis is involved in the development of intestinal permeability, probiotics may help balance the gut microbiota.
One study with animals found that probiotic strains benefited leaky gut in mice, including reducing gut dysbiosis, inflammation, and metabolic dysfunction. The probiotic bacteria also increased tight junctions between epithelial cells.10
Probiotic supplements have also been shown to be beneficial for other digestive disorders, including inflammatory bowel disease (like Crohn’s disease and ulcerative colitis), irritable bowel syndrome, and celiac disease, which could help prevent or improve leaky gut by reducing those gastrointestinal symptoms.
In addition to probiotic pills, increasing dietary probiotics can boost the diversity of beneficial bacteria in the gut microbiome. Dietary probiotics are found in fermented foods, including sauerkraut, kimchi, yogurt, natural pickles, miso, natto, tempeh, kombucha, and kefir.
Other Supplements
A few other supplementary that may help with different aspects of leaky gut include:
- L-glutamine, an amino acid that strengthens the integrity of the intestinal lining
- Zinc, which may reduce gut permeability in people with inflammatory gut conditions like inflammatory bowel disease
- Omega-3 fatty acids, which reduce inflammation and help with dysbiosis
Gluten-Free Diet
Although a gluten-free diet is not needed for everybody, it’s thought to improve leaky gut in people with high genetic susceptibility. Gluten can trigger zonulin activation in some people, which is known to increase the gaps between tight junctions and contribute to leaky gut.
One older study found that 87% of people with celiac disease (who absolutely need to be on a gluten-free diet) had normalization of their increased intestinal permeability after one year of eating gluten-free. Conversely, people who consumed even trace amounts of gluten had increased markers of leaky gut at the next visit.11
Eating Antioxidants and Anti-Inflammatory Foods
If you suspect you have leaky gut and want to heal it through diet, consider consuming foods high in antioxidants, anti-inflammatory foods, and nutrient-dense foods.
Some foods that can help with leaky gut (such as those high in polyphenols) include:
- Berries, apples, pears, pomegranate, and citrus fruit
- Dark leafy greens, cruciferous vegetables (broccoli, kale, Brussels sprouts, cauliflower), and orange or red-colored vegetables
- Salmon, mackerel, anchovies, tuna, and sardines are especially rich in omega-3 fatty acids, which are essential for modulating inflammation.
- Nuts and legumes
- Herbs and spices, especially oregano, rosemary, turmeric, ginger, garlic, cinnamon, parsley, cloves, saffron, and basil
- Green tea and coffee (if tolerated)
Limiting or avoiding foods, drinks, and medications that trigger inflammation is also needed to prevent or treat leaky gut.
Pro-inflammatory foods, beverages, or medications that may cause dysbiosis and damage the intestinal lining include:
- Processed foods high in refined carbohydrates, fat, or sugar, including fast food, chips, crackers, candy, desserts, white bread, and sweets
- Fried food
- High-fructose corn syrup
- Alcohol
- Cigarettes
- Conventional red meat
- Unhealthy fats, like trans fats, margarine, and most seed oils, including corn, canola, and soybean oil.
- NSAIDs and antibiotics
- Artificial dyes, preservatives, and sweeteners
- For some people, gluten and dairy can be inflammatory.
Leaky Gut Syndrome FAQs
What is the single most common trigger that leads to leaky gut syndrome?
There are many potential triggers for leaky gut, with some of the most common being a poor diet high in sugar and unhealthy fat, excessive alcohol consumption, gut dysbiosis (which often comes from an unhealthy diet), and consumption of gluten in sensitive people. These factors can all cause increased intestinal permeability.
Is coffee bad for leaky gut syndrome?
Not necessarily, although it can vary individually. Coffee is full of antioxidants, but some people don’t tolerate it well. Plus, what you add to your coffee is also important—if you add loads of flavorings and sugar, then, yes, your favorite coffee may be bad for leaky gut.
How can I test for leaky gut syndrome?
The main tests for leaky gut are zonulin levels, which are elevated in cases of intestinal hyperpermeability, and the lactulose-mannitol test, which measures the absorption of two different sugars (lactulose and mannitol) through the gut. If high levels of both sugars are found in the urine after drinking the lactulose-mannitol solution, it may indicate increased intestinal permeability. However, tests for leaky gut are not standardized because many doctors do not recognize leaky gut syndrome as a medical diagnosis.
- Fasano A. (2020). All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. F1000Research, 9, F1000 Faculty Rev-69. https://doi.org/10.12688/f1000research.20510.1
- Trøseid, M., Nestvold, T. K., Rudi, K., Thoresen, H., Nielsen, E. W., & Lappegård, K. T. (2013). Plasma lipopolysaccharide is closely associated with glycemic control and abdominal obesity: evidence from bariatric surgery. Diabetes care, 36(11), 3627–3632. https://doi.org/10.2337/dc13-0451
- Harbison, J. E., Roth-Schulze, A. J., Giles, L. C., Tran, C. D., Ngui, K. M., Penno, M. A., Thomson, R. L., Wentworth, J. M., Colman, P. G., Craig, M. E., Morahan, G., Papenfuss, A. T., Barry, S. C., Harrison, L. C., & Couper, J. J. (2019). Gut microbiome dysbiosis and increased intestinal permeability in children with islet autoimmunity and type 1 diabetes: A prospective cohort study. Pediatric diabetes, 20(5), 574–583. https://doi.org/10.1111/pedi.12865
- Buscarinu, M. C., Romano, S., Mechelli, R., Pizzolato Umeton, R., Ferraldeschi, M., Fornasiero, A., Reniè, R., Cerasoli, B., Morena, E., Romano, C., Loizzo, N. D., Umeton, R., Salvetti, M., & Ristori, G. (2018). Intestinal Permeability in Relapsing-Remitting Multiple Sclerosis. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics, 15(1), 68–74. https://doi.org/10.1007/s13311-017-0582-3
- Scher, J. U., Sczesnak, A., Longman, R. S., Segata, N., Ubeda, C., Bielski, C., Rostron, T., Cerundolo, V., Pamer, E. G., Abramson, S. B., Huttenhower, C., & Littman, D. R. (2013). Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. eLife, 2, e01202. https://doi.org/10.7554/eLife.01202
- Sánchez, E., Donat, E., Ribes-Koninckx, C., Fernández-Murga, M. L., & Sanz, Y. (2013). Duodenal-mucosal bacteria associated with celiac disease in children. Applied and environmental microbiology, 79(18), 5472–5479. https://doi.org/10.1128/AEM.00869-13
- Odenwald, M. A., & Turner, J. R. (2013). Intestinal permeability defects: is it time to treat?. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association, 11(9), 1075–1083. https://doi.org/10.1016/j.cgh.2013.07.001
- Meddings, J. B., Jarand, J., Urbanski, S. J., Hardin, J., & Gall, D. G. (1999). Increased gastrointestinal permeability is an early lesion in the spontaneously diabetic BB rat. The American journal of physiology, 276(4), G951–G957. https://doi.org/10.1152/ajpgi.1999.276.4.G951
- Krawczyk, M., Maciejewska, D., Ryterska, K., Czerwińka-Rogowska, M., Jamioł-Milc, D., Skonieczna-Żydecka, K., Milkiewicz, P., Raszeja-Wyszomirska, J., & Stachowska, E. (2018). Gut Permeability Might be Improved by Dietary Fiber in Individuals with Nonalcoholic Fatty Liver Disease (NAFLD) Undergoing Weight Reduction. Nutrients, 10(11), 1793. https://doi.org/10.3390/nu10111793
- Ahmadi, S., Wang, S., Nagpal, R., Wang, B., Jain, S., Razazan, A., Mishra, S. P., Zhu, X., Wang, Z., Kavanagh, K., & Yadav, H. (2020). A human-origin probiotic cocktail ameliorates aging-related leaky gut and inflammation via modulating the microbiota/taurine/tight junction axis. JCI insight, 5(9), e132055. https://doi.org/10.1172/jci.insight.132055
- Duerksen, D. R., Wilhelm-Boyles, C., & Parry, D. M. (2005). Intestinal permeability in long-term follow-up of patients with celiac disease on a gluten-free diet. Digestive diseases and sciences, 50(4), 785–790. https://doi.org/10.1007/s10620-005-2574-0








