This post contains links through which we may earn a small commission should you make a purchase from a brand. This in no way affects our ability to objectively critique the products and brands we review.
What to Know About the New Over-the-Counter CGMs (Continuous Glucose Monitor)
Evidence Based Research To fulfill our commitment to bringing our audience accurate and insightful content, our expert writers and medical reviewers rely on carefully curated research.
Read Our Editorial Policy
Checking blood sugar levels all day with fingerpricks or continuous glucose monitors (CGMs) has typically been reserved for people with type 1 or 2 diabetes.
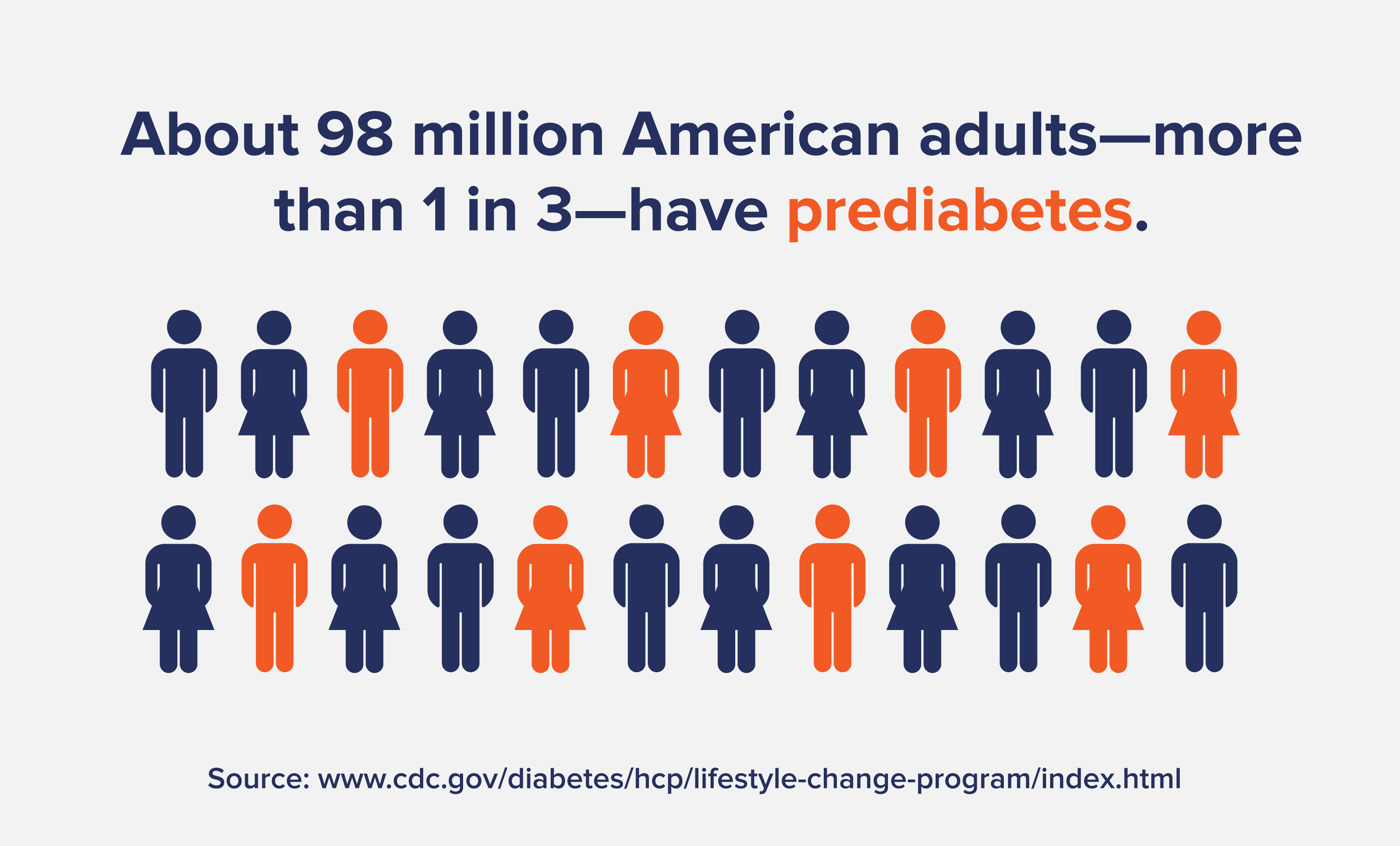
However, with 1 in 3 Americans having prediabetes and only 12% having a healthy metabolic function, it’s becoming more and more critical to keep an eye on rising or unstable blood sugar levels.
Keep reading to learn about how CGMs work, the new over-the-counter versions just released, and the pros and cons for people without diabetes using CGMs.
What Are CGMs?
Continuous glucose monitors (CGMs) are blood sugar monitoring devices that people with diabetes use to manage their blood glucose in real time.
As opposed to the uncomfortable and frequent fingerstick blood readings (where you have to prick your finger to measure sugar in your blood) of the past, CGMs are small monitors that continually measure glucose in the blood.
They’re typically applied to the back of the arm or abdomen and have a sensor, transmitter, and receiver. The sensor measures the glucose levels of the fluid surrounding your cells, which is a good proxy for blood glucose. The sensor then wirelessly transmits data to a receiver (typically a smartphone), where you can see real-time blood sugar readings.
This is a vast improvement above painful fingerprick readings, which people with diabetes must do multiple times daily.
However, while CGM sensors are durable and don’t need to be removed while exercising, showering, or sleeping, they don’t last too long, needing to be replaced every two weeks or so.
A Look at the First Dexcom Over-the-Counter CGM
Dexcom has recently released the first over-the-counter (OTC) CGM for people with or without diabetes.
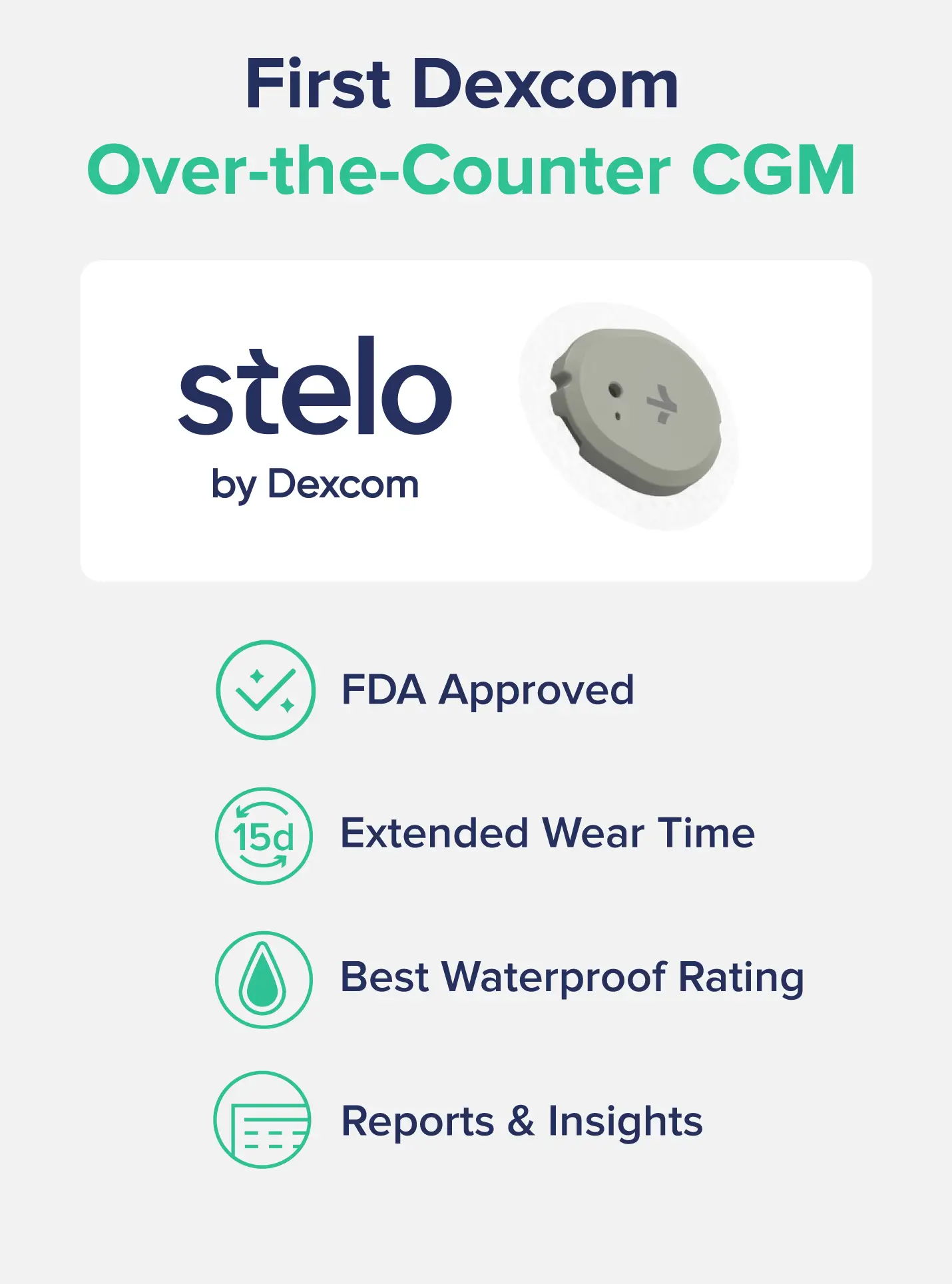
Dexcom has released and received FDA approval for the Stelo device, a CGM targeted for people who do not use insulin. Although it’s designed for people with type 2 diabetes who don’t use insulin, it can also be used by people with prediabetes or no metabolic diagnoses.
It offers the longest biosensor wear time (15 days) and the best waterproof rating. Dexcom Stelo’s sensor also provides daily, weekly, and session summary insights, blood sugar spikes, and pattern detection.
Dexcom Stelo is not covered by insurance and is available for $99 a month or $89 per month with a subscription.
The FDA has recently cleared two other OTC CGMs—Abbott’s Lingo and Libre Rio. Like Dexcom Stelo, the Libre Rio is designed for people with type 2 diabetes who don’t use insulin. On the other hand, the Lingo is more of a wellness device intended for health-conscious consumers to monitor their blood sugar and metabolic health without diagnosing any conditions. However, Lingo has a waitlist at the time of this writing.
Lingo is very similar to Levels, another wellness-focused CGM that now offers Dexcom as its prescription-free version (with a very high cost of $199/month and an additional $199 annual fee)
Benefits and Downsides of Using a CGM
Although most people intuitively understand that chugging a Big Gulp full of Dr. Pepper or mowing down a family-size bag of Skittles can elevate blood sugar, many other seemingly innocuous (and healthy) foods can also raise blood sugar. This is one reason why CGMs can be helpful for people without diabetes.
Some people respond much better to carb-dominant foods than others. For example, you may not see a huge blood sugar rise when you eat a bowl of oatmeal, while someone else could have a spike through the roof that impacts how they feel. Learning your own triggers for blood sugar spikes can be helpful, especially if you often feel sluggish or low-energy throughout the day.
That said, not everybody should use a CGM—especially people with a history of disordered eating. Checking your blood sugar constantly and only eating foods that don’t impact blood sugar can become a form of obsessive or disordered eating.
It’s also important to know that having blood sugar spikes is a normal part of eating food. It’s not always the bad spike, but how well your body responds to it and can get your blood sugar back to normal levels.
For example, if you snack on a bowl of delicious late summer strawberries, your blood sugar will probably spike shortly after due to the influx of sugar.
However, if you then see a subsequent drop back to normal levels, that’s not a problem—your body is effectively using insulin to shuttle the sugar out of your blood and into cells for energy or storage. Conversely, if your blood sugar stays elevated for hours afterward, that’s a sign you are having metabolic problems like insulin resistance. This means that the insulin isn’t working the way it should, and sugar is remaining in your blood.
Overall, if you do not have prediabetes or diabetes (type 1 or type 2) or a history of disordered eating, using a CGM for a short period (a month or two) can be a beneficial way to see how well your body responds to eating carbohydrates. It can also help show you which foods are causing blood sugar spikes in your metabolism and pinpoint triggers that cause symptoms like low energy, sluggishness, or crashes from rollercoaster-like blood sugar curves.