This post contains links through which we may earn a small commission should you make a purchase from a brand. This in no way affects our ability to objectively critique the products and brands we review.
How Much Vitamin D Do You Get From the Sun?
Evidence Based Research To fulfill our commitment to bringing our audience accurate and insightful content, our expert writers and medical reviewers rely on carefully curated research.
Read Our Editorial Policy
There’s a reason why vitamin D is nicknamed “the sunshine vitamin,” as the best natural vitamin D sources is the sun.
Vitamin D is a vital micronutrient many people lack. Its benefits include healthy bones, metabolic function, cognition, heart health, immune health, and more. The simplest way to get it is through moderate sunlight exposure.
However, there are some caveats to consider and many factors that affect vitamin D synthesis—let’s take a closer look at how much vitamin D you can safely get from the sun.
Your Body, Evidence-Based
Skip forums—get answers tailored to you in 45 minutes.
Your Body, Evidence-Based
Skip forums—get answers tailored to you in 45 minutes.

How Do We Make Vitamin D From the Sun?
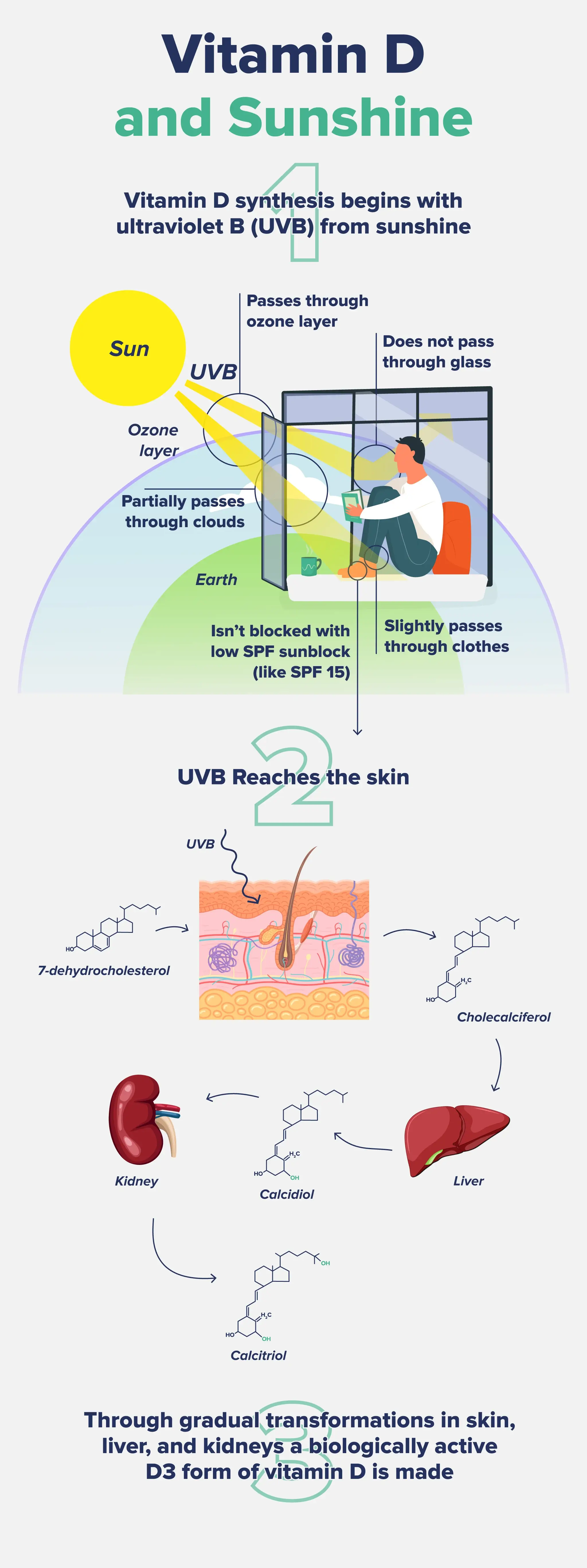
We synthesize vitamin D when our skin is exposed to UVB (ultraviolet B) rays from the sun (or artificial UVB lamps).
For a quick nutritional biochemistry lesson, a form of cholesterol called 7-dehydrocholesterol in the plasma membranes of skin cells (epidermal keratinocytes and dermal fibroblasts) absorbs UVB photons upon sunlight exposure.1
The addition of UVB causes 7-dehydrocholesterol to transform into an inactive form of vitamin D called pre-vitamin D3 or precalciferol.1
Previtamin D3 converts into vitamin D3 (cholecalciferol), which is then metabolized in the liver to 25-hydroxyvitamin D3 (the circulating form found in the blood), then in the kidneys to its biologically active form, 1,25-dihydroxyvitamin D3.1 As we don’t get much vitamin D from our food intake, sunlight is the primary method for boosting or maintaining its levels, and people who get more sun exposure have higher blood vitamin D levels than people who spend more time inside.2
How Much Vitamin D Do You Make From the Sun?
The short (and annoying) answer is: it depends.
As we’ll see in the next section, many factors can impact vitamin D synthesis, most of which are outside our control.
Let’s take a look at some studies that have assessed vitamin D production from sunshine exposure.
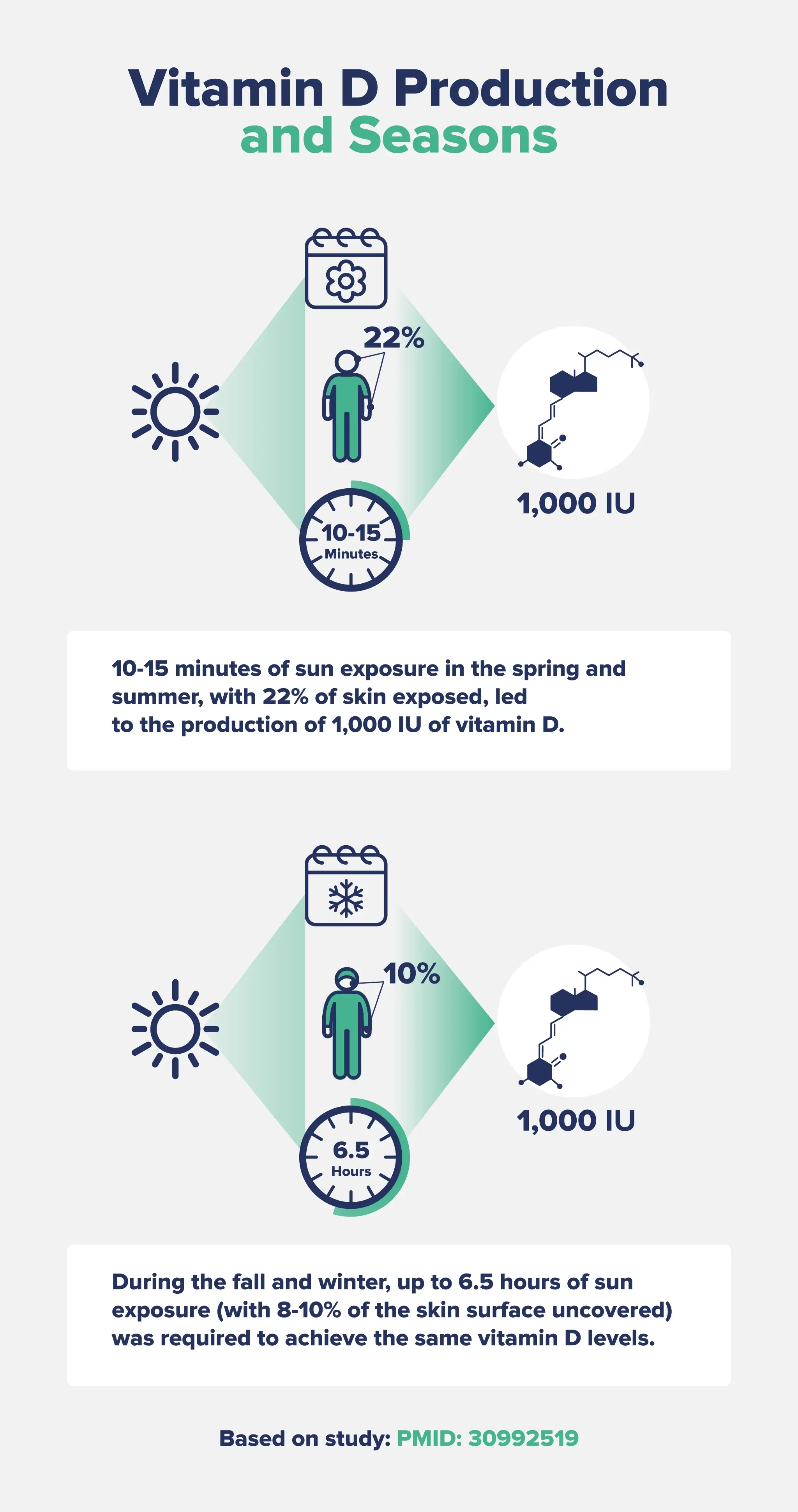
First, a study in Switzerland found that just 10-15 minutes of sun exposure in the spring and summer, with 22% of skin exposed, led to the production of 1,000 IU of vitamin D.3
During these warmer seasons, the time between sunburn risk and producing 1,000 IU of vitamin D ranged from 9 to 46 minutes. This means that some people are at a greater risk of developing harmful sunburns before they reach adequate vitamin D production.3
During the fall and winter, up to 6.5 hours of sun exposure (with 8-10% of the skin surface uncovered) was required to achieve the same vitamin D levels, which increases the risk of sunburn or sun damage.3
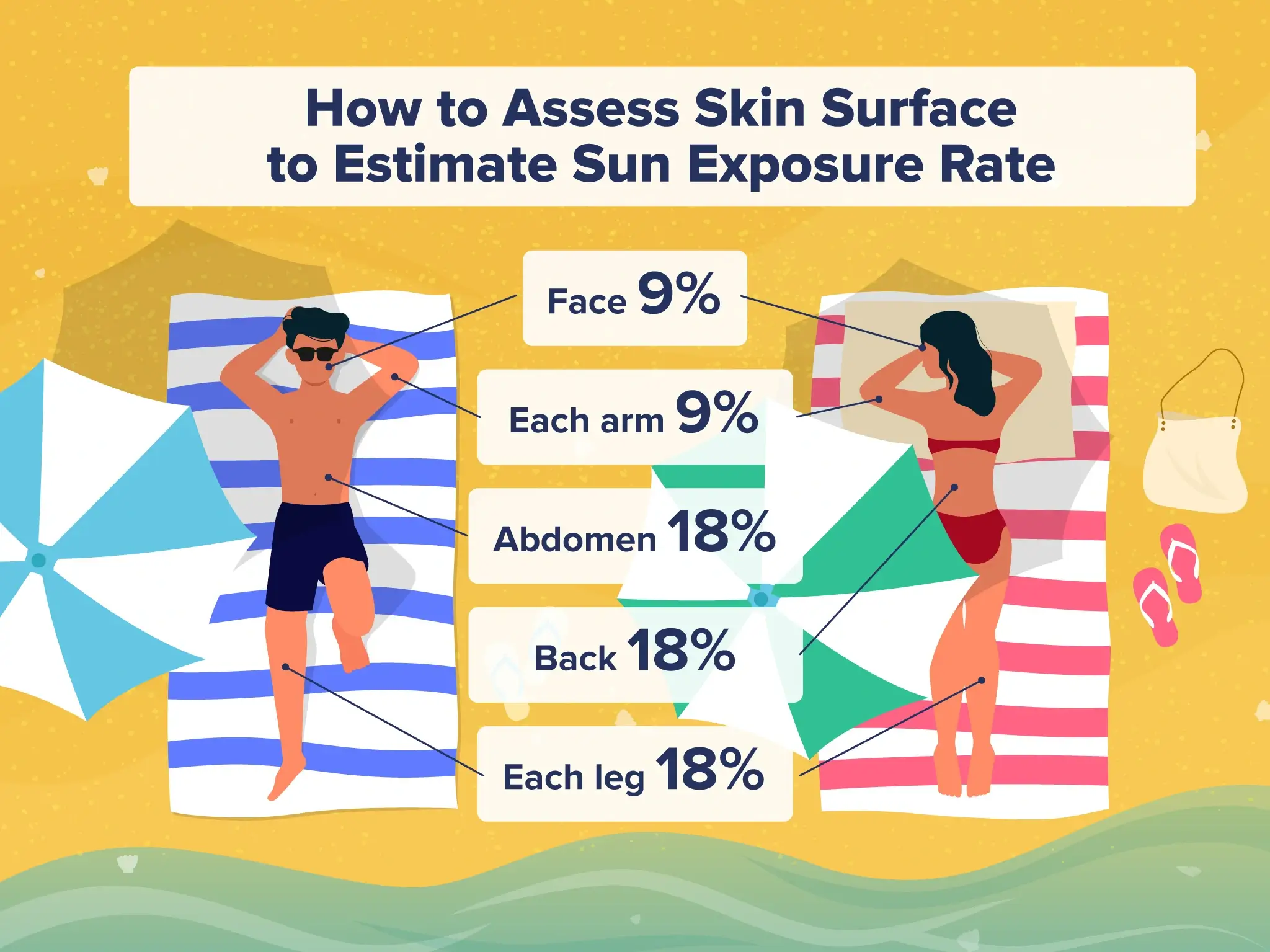
For reference, the face accounts for approximately 9% of the body’s surface, each arm is 9%, each leg is 18%, and the abdomen and back are 18% each.
Sunnier environments accelerate vitamin D synthesis, allowing the body to produce ~1,000 IUs within just a few minutes.4
It’s generally recommended that you expose yourself to sunlight for 50% of the time it would take you to develop a mild sunburn or slight pinkness that remains 24 hours later—this is called the “minimal erythemal dose,” or MED.4
Exposing the whole body (like in a bathing suit) to 0.5 MED of UVB radiation (meaning it did not cause sunburn) has been shown to synthesize 7,000 to 10,000 IU of vitamin D.4
As everyone’s MED is different, the time this takes would vary depending on how quickly you tend to burn.
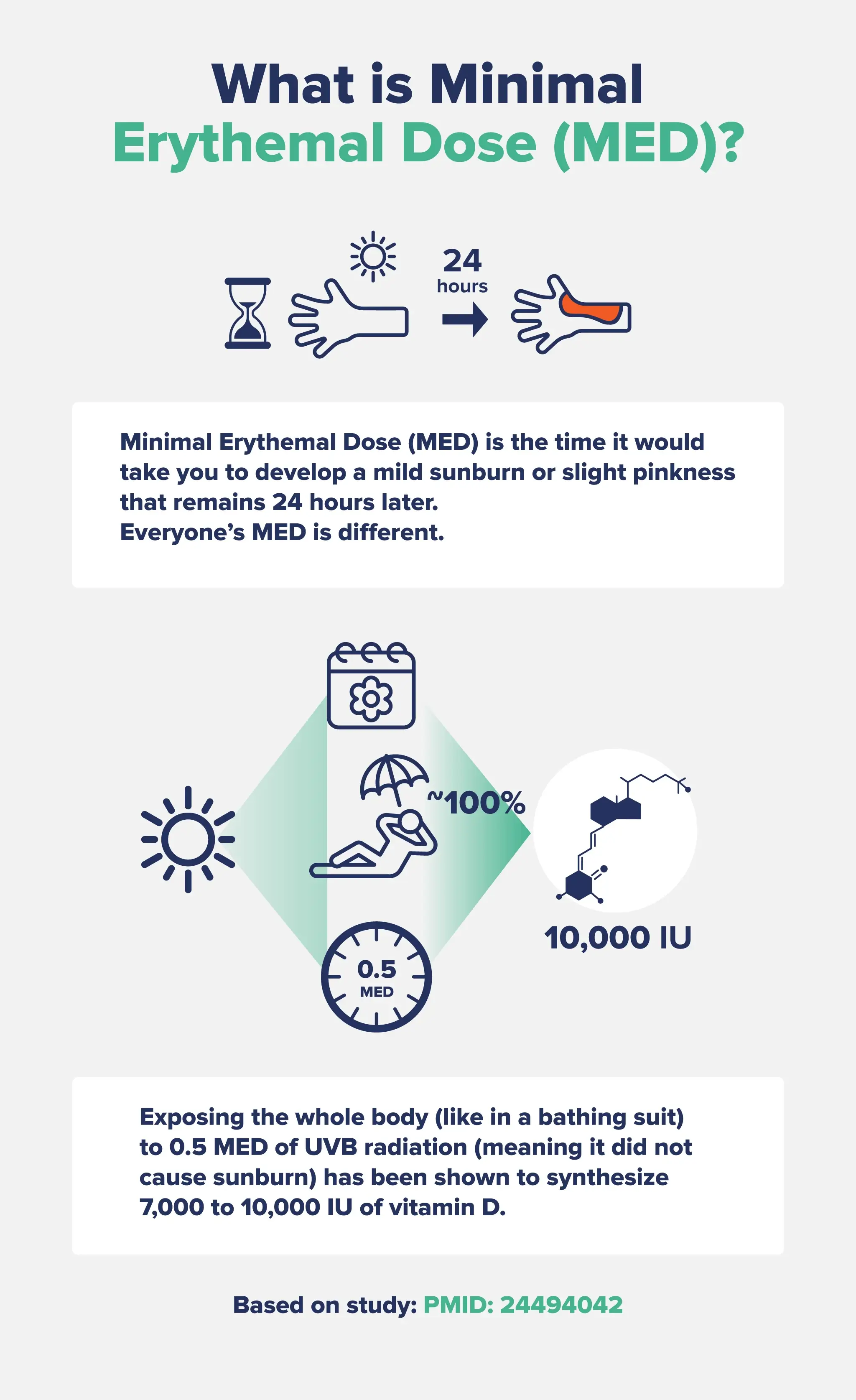
Research has shown that fair-to-medium-skinned adults in bathing suits who were exposed to 0.5 MED of UV radiation just once per week for 3 months increased their serum vitamin D levels by 125-200%. In comparison, adults who took 1,000 IU of supplemental vitamin D daily during that time increased their blood levels by about 50%.5
This study in Australia found that summertime sun exposure for 2 to 14 minutes at noon (three to four times per week with 15% of the body exposed) produced up to 600 IU of vitamin D (the Recommended Dietary Allowance) in fair-skinned people.6
However, sunburn was found to occur in as little as 8 minutes—again, meaning that some people might not get enough vitamin D without burning first.6
To circumvent this, some researchers recommend getting sunshine “little and often,” which could mean 5 minutes of exposure at a time, a few times daily.

In the winter, when perhaps only your face and hands are exposed, it may take up to 6 hours of sun exposure during peak hours for your skin to produce sufficient vitamin D, which is why a vitamin D supplement is often recommended during the cooler months.3
Overall, it’s estimated that 5 to 15 minutes of sun exposure with 25% or more of your body exposed at least three times a week during peak hours (11 a.m. to 3 p.m.) is likely adequate to maintain healthy blood vitamin D levels. If you have dark skin, you may need up to 30 minutes.
That said, many factors affect how much vitamin D our skin can make—let’s take a closer look.
Factors That Affect Vitamin D Synthesis

Geographic Location
People living in more northern latitudes farther away from the equator have lower exposure to the sun.4
This is due to something called the “solar zenith angle.”
The solar zenith angle is the angle between the local zenith (directly above the point where you are on the ground) and the line of sight from that point to the sun. The higher the sun is in the sky and the closer to the equator you are, the lower the solar zenith angle.4
As the solar zenith angle increases (when the sun gets further away from the highest point in the sky), the amount of UVB rays reaching the earth’s surface is reduced. At higher latitudes—which have a greater distance from the equator—more UVB radiation is absorbed by the ozone layer, meaning it’s less able to reach our skin.4
In general, the further you get from the equator, the lower the vitamin D status of that population.
At high latitudes (>40°), the sun does not provide any vitamin D during the winter, making vitamin D supplements, cod liver oil, or a focus on consuming fatty fish essential.7
For example, people living in Boston (42° North), Edmonton, Canada (52° North), Norway (60° North), and Ushuaia, Argentina (55° South) are all unable to produce significant amounts of vitamin D from the sun for 4 to 6 months of the year.4
Skin Color and Type
How much vitamin D you make has a lot to do with your skin color and type. Skin type is based on the Fitzpatrick scale:
- Type I: The palest and whitest skin tone that always burns (and quickly) and never tans
- Type II: Fair/white and usually burns; sometimes tans, but with difficulty
- Type III: Medium, white/olive skin tone; sometimes mildly burns but gradually tans into an olive color
- Type IV: Olive/moderate brown; rarely burns and tans easily
- Type V: Brown/dark brown; very rarely burns and tans very easily
- Type VI: Black/very dark brown; never burns and tans very easily
People with Type IV (sometimes Type III) and above have more melanin in their skin, which helps to protect the skin against damage from excessive sun. Melanin absorbs UV rays, acting like an internal sunscreen. (However, this does not mean people with darker skin are immune to skin cancer!)8
While it’s helpful that people with dark skin types don’t burn as quickly, that also means that they don’t produce vitamin D as easily.
Some research suggests that people with darker skin need anywhere from 30 minutes to 2 hours longer in the sun than light-skinned people to get the same amount of vitamin D.8
Season and Time of Day
Both the time of year and the time of day affect vitamin D synthesis, which is again related to the sun’s solar zenith angle.
The solar zenith angle is increased during the early morning and late afternoon (when the sun is not directly overhead) and during the winter months.4
The best vitamin D synthesis comes at midday, but peak hours are from 10 am to 2 pm. The UV Index needs to be over 3 for our skin to produce significant vitamin D, which often only occurs during these midday hours. In the summer, the peak hours might be extended.4
When the UV index is 3 or higher, these are the general recommendations for the maximum amount of time to expose unprotected skin:9
- Type I: 10 minutes
- Type II: 20 minutes
- Type III: 30 minutes
- Type IV: 50 minutes
- Type V and VI: 60 minutes
Overall, midday summer sun exposure will produce the fastest and most significant vitamin D synthesis.
Clothing
The more clothing you wear or cover your body with, the less surface area is exposed to the sun’s UVB rays.
Although it seems straightforward, there are some caveats here, too. As you may know, if you spend a lot of time outdoors, some clothing is equipped with UPF (UV Protection Factor), while others are not.
If you are wearing UPF clothing, UVB rays will not penetrate the clothing and you will not make vitamin D under the covered areas.
However, some fabrics do let through some UVB rays. For example, a 2014 study found that 100% cotton-knitted fabric allowed for a 15% transmittance of solar UV rays, leading to a slower rate of vitamin D synthesis with reduced sunburn risk.10
If you want to make the most out of your 5-30 minutes in the sun, take off as many clothes as reasonably possible (and appropriate!) to get the maximum amount of vitamin D synthesis.
Weight
Excess body weight may affect how the body synthesizes and stores vitamin D.
Research has found that obese people have a 57% lower vitamin D synthesis after exposure to both whole-body UV radiation and high-dose vitamin D supplementation compared to people with non-obese BMIs.11
Although the research isn’t conclusive, one reason might be that subcutaneous adipose tissue has lower expression of one of the enzymes needed to convert inactive vitamin D into its active form.12
This means that people with more adipose tissue (fat) may have trouble with the conversion process that fully activates vitamin D.
Genetics
Researchers have pinpointed several genes that are involved in the synthesis and transport pathways related to vitamin D metabolism.13
Alterations or variants in these genes may affect overall vitamin D status, including how it’s synthesized in the skin.
One of the genetic variants involved in vitamin D synthesis is the gene DHCR7 (7-Dehydrocholesterol Reductase).14
If you recall from our biochem lesson earlier, 7-dehydrocholesterol is the form of cholesterol in our skin that reacts with UVB rays to start the vitamin D synthesis process.
DHCR7 encodes for the enzyme that helps the conversion of 7-dehydrocholesterol into cholesterol. People with elevated expression of this gene will have increased rates of this conversion, which reduces the availability of 7-dehydrocholesterol in the skin for UVB rays to interact with.14
Other genes may also be altered, including those related to vitamin D receptors, vitamin D binding proteins, transport proteins, and cholesterol metabolism.14
Sunscreen Use
Some researchers think that the rise in sunscreen use over the past 50 or so years is a leading reason why vitamin D deficiency is so prevalent in modern society.15
Conversely, other researchers state that sunscreen typically does not significantly inhibit vitamin D synthesis (which may be in part because people apply sunscreen so poorly).16
While sunscreen is undoubtedly essential to protect against skin cancer and sun damage, there is a middle ground many of us can take to optimize our vitamin D synthesis while still protecting ourselves.
Most studies have used a lower SPF (like SPF 15), which still allows for some vitamin D production. It’s also important to note that only broad-spectrum sunscreen (that blocks both UVA and UVB rays) would affect vitamin D, as we only make it in our skin upon exposure to UVB.
The authors of a review in the British Journal of Dermatology conclude, “Judicious use of daily broad‐spectrum sunscreens with high ultraviolet (UV) A protection will not compromise vitamin D status in healthy people.”17
However, they also state that people using high-SPF sunscreens, protective clothing, or shade-seeking behavior are more likely to have compromised vitamin D status.
Other research states that sunscreens with an SPF of 30 will absorb approximately 95% of incident UVB radiation, reducing vitamin D production in the skin by about 95%.15
Overall, a moderate broad-spectrum sunscreen with higher UVA protection (~SPF 15) will likely not affect vitamin D synthesis, and daily sunscreen is always recommended to protect against skin cancer, skin damage, and premature aging.
That said, getting 5-30 minutes of unprotected sunlight exposure (depending on your skin type and propensity to burn) without sunscreen is the best way to raise vitamin D levels. If you are worried about premature aging, always apply sunscreen to your face and instead use your arms.
Vitamin D and Sun FAQs
Is sunlight better than vitamin D supplements?
Research shows that vitamin D levels are higher when people are exposed to sunlight than when they take vitamin D supplements. High-dose vitamin D might be an exception in cases of vitamin D deficiency, but sunlight is generally better at raising vitamin D status.
How much sunlight time do you need to raise vitamin D?
It depends on many factors, including your skin tone, geographic location, time of year, time of day, genetics, and weight. On average, about 10 to 15 minutes of mid-day sun exposure (with 25% or more of your skin exposed—like your arms, face, and neck, for example—is sufficient to produce about 1,000 IU of vitamin D. If you have darker skin, live in a more northern latitude, are wearing more clothes or coverings, or if it’s cloudy out, more time may be needed. Conversely, if you have lighter skin types, you may only need (or be able to) stay in the sun for 5 minutes.
How can I raise my vitamin D level quickly?
Sunshine is the best way to increase your vitamin D status fast. About 10 to 15 minutes of mid-day sun with about 25% or more of your skin exposed is typically adequate to produce 1,000 IU of vitamin D, which is more than the RDA. High-dose supplements can also raise your vitamin D levels rapidly. Talk with your doctor and check your blood vitamin D levels before using high-dose vitamin D supplementation.
Do you get vitamin D when it’s cloudy?
Just like how you can get sunburned when it’s cloudy out, you can still produce vitamin D in your skin. However, it will be a lower rate compared to when it’s bright and sunny out. UV light is still present through the clouds, but the UV Index typically needs to be above 3 for significant vitamin D synthesis.
Does sunscreen block vitamin D?
The research is conflicting here. Most studies show that a broad-spectrum sunscreen with a low SPF (like SPF 15) does not affect vitamin D synthesis. However, many people do not apply sunscreen correctly (which may skew study results) and also use sunscreen with much higher SPF. Generally, just 5 to 30 minutes every few days (depending on skin type) of unprotected sun exposure in the warmer months is enough to maintain optimal vitamin D levels.
Can you get vitamin D through windows?
No, you cannot get vitamin D through a window. Window glass blocks UVB rays, and we synthesize vitamin D in our skin only upon exposure to UVB rays.
Do you get vitamin D in the shade?
It depends on how much shade you are in. If you are completely blocked from all sunlight, you cannot make vitamin D. However, if it’s partial shade or dappled shade (like under a tree), you can make some. Research has shown that UVB wavelengths under a shade umbrella or under a tree were at 52% and 55% of the levels found in complete sunshine, respectively.18 This means that partial shade cuts the available UVB by about half, meaning it would take about twice as long to produce the same vitamin D as when you’re in the full sun.
What foods have vitamin D?
Not that many foods naturally contain vitamin D. The best dietary sources are fatty fish (like wild salmon, mackerel, sardines, tuna, and halibut), cod liver oil, egg yolks, some mushrooms, and fortified foods like orange juice, fortified cereals, and milk.
- Bikle DD. Vitamin D: Production, Metabolism and Mechanisms of Action. [Updated 2021 Dec 31]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278935/
- Brouwer-Brolsma, E. M., Vaes, A. M. M., van der Zwaluw, N. L., van Wijngaarden, J. P., Swart, K. M. A., Ham, A. C., van Dijk, S. C., Enneman, A. W., Sohl, E., van Schoor, N. M., van der Velde, N., Uitterlinden, A. G., Lips, P., Feskens, E. J. M., Dhonukshe-Rutten, R. A. M., & de Groot, L. C. P. G. M. (2016). Relative importance of summer sun exposure, vitamin D intake, and genes to vitamin D status in Dutch older adults: The B-PROOF study. The Journal of steroid biochemistry and molecular biology, 164, 168–176. https://doi.org/10.1016/j.jsbmb.2015.08.008
- Religi, A., Backes, C., Chatelan, A., Bulliard, J. L., Vuilleumier, L., Moccozet, L., Bochud, M., & Vernez, D. (2019). Estimation of exposure durations for vitamin D production and sunburn risk in Switzerland. Journal of exposure science & environmental epidemiology, 29(6), 742–752. https://doi.org/10.1038/s41370-019-0137-2
- Wacker, M., & Holick, M. F. (2013). Sunlight and Vitamin D: A global perspective for health. Dermato-endocrinology, 5(1), 51–108. https://doi.org/10.4161/derm.24494
- Holick M. F. (2008). Vitamin D and sunlight: strategies for cancer prevention and other health benefits. Clinical journal of the American Society of Nephrology : CJASN, 3(5), 1548–1554. https://doi.org/10.2215/CJN.01350308
- Samanek, A. J., Croager, E. J., Gies, P., Milne, E., Prince, R., McMichael, A. J., Lucas, R. M., Slevin, T., & Skin Cancer Prevention (2006). Estimates of beneficial and harmful sun exposure times during the year for major Australian population centres. The Medical journal of Australia, 184(7), 338–341. https://doi.org/10.5694/j.1326-5377.2006.tb00267.x
- Cicarma, E., Porojnicu, A. C., Lagunova, Z., Dahlback, A., Juzeniene, A., & Moan, J. (2009). Sun and sun beds: inducers of vitamin D and skin cancer. Anticancer research, 29(9), 3495–3500.
- Raymond-Lezman, J. R., & Riskin, S. I. (2023). Benefits and Risks of Sun Exposure to Maintain Adequate Vitamin D Levels. Cureus, 15(5), e38578. https://doi.org/10.7759/cureus.38578
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. How much sun is too much? 2011 Jul 22 [Updated 2018 Nov 29]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK321117/
- Piotr S. Sobolewski, Janusz W. Krzyścin, Janusz Jarosławski, Jakub Wink, Aleksandra Lesiak, Joanna Narbutt. Controlling adverse and beneficial effects of solar UV radiation by wearing suitable clothes – Spectral transmission of different kinds of fabrics, Journal of Photochemistry and Photobiology B: Biology, Volume 140, 2014, Pages 105-110, https://doi.org/10.1016/j.jphotobiol.2014.07.009
- Wortsman, J., Matsuoka, L. Y., Chen, T. C., Lu, Z., & Holick, M. F. (2000). Decreased bioavailability of vitamin D in obesity. The American journal of clinical nutrition, 72(3), 690–693. https://doi.org/10.1093/ajcn/72.3.690
- Vanlint S. (2013). Vitamin D and obesity. Nutrients, 5(3), 949–956. https://doi.org/10.3390/nu5030949
- Das, S., Hasan, M. M., Mohsin, M., Jeorge, D. H., Rasul, M. G., Khan, A. R., Gazi, M. A., & Ahmed, T. (2022). Sunlight, dietary habits, genetic polymorphisms and vitamin D deficiency in urban and rural infants of Bangladesh. Scientific reports, 12(1), 3623. https://doi.org/10.1038/s41598-022-07661-y
- Wang, T. J., Zhang, F., Richards, J. B., Kestenbaum, B., van Meurs, J. B., Berry, D., Kiel, D. P., Streeten, E. A., Ohlsson, C., Koller, D. L., Peltonen, L., Cooper, J. D., O’Reilly, P. F., Houston, D. K., Glazer, N. L., Vandenput, L., Peacock, M., Shi, J., Rivadeneira, F., McCarthy, M. I., … Spector, T. D. (2010). Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet (London, England), 376(9736), 180–188. https://doi.org/10.1016/S0140-6736(10)60588-0
- Holick M. F. (2011). Vitamin D: a d-lightful solution for health. Journal of investigative medicine : the official publication of the American Federation for Clinical Research, 59(6), 872–880. https://doi.org/10.2310/JIM.0b013e318214ea2d
- Neale, R. E., Khan, S. R., Lucas, R. M., Waterhouse, M., Whiteman, D. C., & Olsen, C. M. (2019). The effect of sunscreen on vitamin D: a review. The British journal of dermatology, 181(5), 907–915. https://doi.org/10.1111/bjd.17980
- Passeron, T., Bouillon, R., Callender, V., Cestari, T., Diepgen, T. L., Green, A. C., van der Pols, J. C., Bernard, B. A., Ly, F., Bernerd, F., Marrot, L., Nielsen, M., Verschoore, M., Jablonski, N. G., & Young, A. R. (2019). Sunscreen photoprotection and vitamin D status. The British journal of dermatology, 181(5), 916–931. https://doi.org/10.1111/bjd.17992
- Turnbull, D. J., Parisi, A. V., & Kimlin, M. G. (2005). Vitamin D effective ultraviolet wavelengths due to scattering in shade. The Journal of steroid biochemistry and molecular biology, 96(5), 431–436. https://doi.org/10.1016/j.jsbmb.2005.04.039








